Traumatic brain injury emerges as a distinct and often life-altering experience. It casts a long shadow over one's health, and the journey doesn’t end after hospitalization and discharge. Rather, it introduces a new chapter—one that holds profound implications for cognitive health.
Read on below as we unravel the complexities of TBI and discuss the significance of the hospitalization phase and its link to the risk of dementia.
Traumatic brain injury (TBI) refers to a disruption in normal brain function resulting from an external force. This force can be caused by various incidents, such as accidents, falls, or sports injuries.
From mild concussions to severe brain trauma, the spectrum of TBI is vast, encompassing a range of physical and cognitive consequences, such as:
The severity of traumatic brain injury is a significant factor that can impact the risk of dementia. Research studies have consistently shown that individuals who experience a moderate to severe TBI are at a higher risk of developing dementia later in life compared to those with mild or no TBI.
The gravity of TBI extends beyond the initial incident, with hospitalization playing a pivotal role in the trajectory of recovery. During this phase, medical professionals address immediate concerns, from stabilizing patients to monitoring vital signs.
However, it is not just about the physical recuperation; TBI hospitalization sets the stage for potential cognitive issues that may emerge in the weeks, months, or even years following the injury.
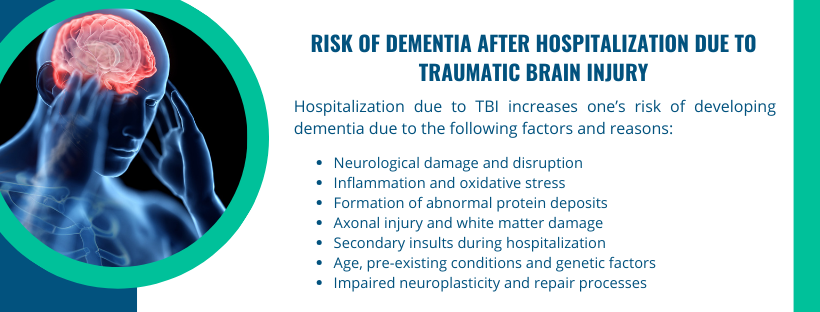
The increased risk of dementia after hospitalization due to TBI is a complex phenomenon with multiple contributing factors. While the exact mechanisms are not fully understood, several vital factors may help explain the heightened risk:
The primary factor contributing to the increased risk is the extent of neurological damage and disruption caused by the traumatic brain injury itself. Severe TBIs can result in significant damage to brain tissue and neural connections.
Traumatic brain injury triggers an inflammatory response in the brain, leading to increased production of pro-inflammatory cytokines.
Chronic inflammation, along with oxidative stress, contributes to ongoing damage and may set the stage for neurodegenerative processes associated with dementia.
TBI has been linked to the accumulation of abnormal proteins in the brain, such as tau and beta-amyloid. These protein deposits are also characteristic of neurodegenerative disorders like Alzheimer's disease, a common cause of dementia.
TBI often involves axonal injury, affecting the long projections of nerve cells responsible for communication between different parts of the brain. White matter damage from TBI can disrupt neural connectivity and contribute to cognitive impairment.
While hospitalization is crucial for the initial management of TBI, certain aspects of the hospital environment may contribute to additional stress on the brain.
Secondary insults, such as complications during surgery, infections, or issues related to intensive care, can exacerbate the overall impact on brain function.
Age at the time of injury is a significant modifier of dementia risk. Older individuals are generally more vulnerable to the long-term effects of TBI. Hospitalized older adults may experience challenges in recovery and may be more susceptible to cognitive decline.
Individuals with pre-existing health conditions or a genetic predisposition to neurodegenerative diseases may face an elevated risk of dementia following TBI. The interaction between TBI and existing vulnerabilities can amplify the overall risk.
TBI can impair neuroplasticity, the brain's ability to reorganize and adapt. This may hinder the brain's natural repair processes, making it more challenging for the neural network to recover and protect against cognitive decline.
While the risk of dementia after traumatic brain injury is a concern, some strategies and interventions can be implemented to potentially mitigate this risk and support cognitive health. Here are several approaches to consider:
Prompt initiation of rehabilitation and treatment following TBI can be crucial. Physical, occupational, and speech therapy, tailored to the individual's needs, can aid recovery and minimize long-term cognitive consequences.
Cognitive rehabilitation focuses on improving specific cognitive functions affected by TBI, such as memory, attention, and problem-solving. These programs aim to enhance neural plasticity and functional recovery.
Additionally, keeping the brain engaged through mentally stimulating activities can support cognitive function. Activities such as puzzles, games, and learning new skills contribute to maintaining cognitive reserves.
Regular physical exercise has been associated with cognitive benefits. It promotes overall brain health, improves blood flow, and supports neuroplasticity. Individuals recovering from TBI should engage in appropriate and supervised exercise programs.
Adopting a healthy lifestyle is crucial. This includes maintaining a balanced diet, staying hydrated, getting sufficient sleep, and avoiding substance abuse. These factors contribute to overall well-being and may positively impact cognitive health.
Regular check-ups and follow-up care with physicians are vital. Ongoing monitoring allows for the identification of any emerging issues and ensures timely intervention.
While the above-mentioned strategies can contribute to mitigating the risk of dementia, it's important to consult specialists for personalized advice and guidance based on individual circumstances.
Are you or a loved one on the path to recovery after a traumatic brain injury?
At NeuLife, we understand that the journey to healing is unique, and we're here to offer comprehensive post-acute rehabilitation to empower individuals facing TBI, spine injuries, amputations, serious orthopedic injuries, strokes, and neurological disorders.

Consult with our experienced physicians and physical therapists at NeuLife to explore personalized strategies aimed at mitigating the risk of dementia post-TBI.
Our team is dedicated to staying at the forefront of rehabilitation science, ensuring you receive the latest and most effective interventions.
Take the first step towards a brighter future. Contact us now at 352-675-2059 or visit our neuro rehab facility!
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.

We know that choosing the next step in your recovery from a catastrophic illness or injury is complex. Together, we can help you take the next step.
Contact us with any questions today.