The cerebellum may be small, but it plays a significant role in moving, balancing, and coordinating our actions. When this vital part of the brain is damaged, simple tasks like walking or speaking can become challenging. Whether caused by injury, illness, or neurological conditions, cerebellar brain damage can significantly impact a person’s daily life.
In this blog, we’ll discuss the common causes of cerebellum damage, the symptoms to watch for, and, most importantly, how rehabilitation can help individuals regain control, rebuild strength, and reclaim independence.
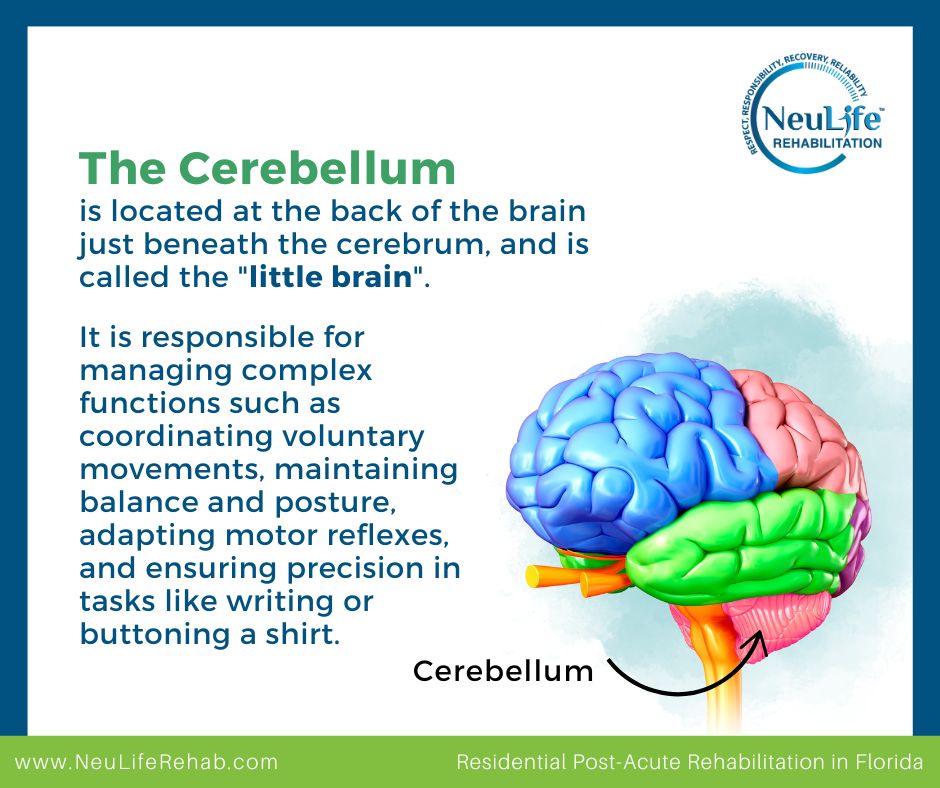
The cerebellum, located at the back of the brain just beneath the cerebrum, is Latin for "little brain"—but don’t let the name fool you. It handles complex tasks essential to moving smoothly and reacting appropriately to our environment. This includes:
Traumatic Brain Injury (TBI) can impact different areas of the brain, with effects varying based on injury location and severity. Commonly affected regions include the cerebrum (which governs cognitive functions, motor skills, and emotions), the cerebellum (responsible for balance and coordination), and the brainstem (which controls vital functions like breathing and heart rate). TBI can result in physical, cognitive, and emotional changes, so early diagnosis and treatment are essential for optimal recovery.
To learn more, read our blog on “What Parts of the Brain Are Impacted by TBI?”
The importance of understanding cerebellum damage goes beyond the surface—here’s what you should know:
Recognizing the signs of cerebellum damage, such as unsteady movement (ataxia), slurred speech, difficulty with coordination, or balance issues, can lead to quicker diagnosis and intervention. The earlier the damage is addressed, the more effective rehabilitation tends to be.
Because the cerebellum doesn’t control cognition or speech like the cerebrum, its damage might not always be immediately recognized. Misdiagnoses or delays in treatment can worsen the long-term impact. Awareness helps ensure that this critical part of the brain isn’t ignored.
While cerebellum damage primarily affects motor control, it can also lead to subtle cognitive and emotional changes, such as difficulty with planning, memory, or emotional regulation. This condition, called Cerebellar Cognitive Affective Syndrome (CCAS), is still being actively researched and is often missed in clinical evaluations.
Understanding the nature of cerebellum damage helps shape effective rehabilitation programs. For example:
Knowledge reduces fear. When patients and caregivers understand cerebellum brain damage, they’re better prepared to manage symptoms, engage in therapy, and make informed care decisions. It fosters realistic expectations and promotes proactive involvement in the recovery process.
Several factors can lead to damage in the cerebellum, including:
Accidents or blows to the head can damage the cerebellum, leading to difficulty with coordination and motor control.
A stroke in the cerebellum, usually caused by a blockage or rupture of blood vessels, can result in severe movement issues.
Chronic alcohol consumption can impair cerebellum function, resulting in ataxia (loss of coordination).
Brain tumors, especially those located in or near the cerebellum, can interfere with their function, leading to coordination problems.
Meningitis or encephalitis can cause inflammation in the brain, potentially affecting the cerebellum.
Conditions like multiple sclerosis (MS), Parkinson’s disease, or spinocerebellar ataxia can progressively damage the cerebellum over time.
Damage to the cerebellum can result in a variety of symptoms, such as:
Rehabilitation is crucial in assisting individuals with cerebellum damage to recover as much function as possible. A post-acute rehabilitation center like NueLife Rehabilitation focuses on helping patients regain lost abilities and enhance their overall quality of life.
The rehabilitation process typically includes:
Below are key strategies for effectively managing cerebellum damage over the long term.
Recovery from cerebellar brain damage varies depending on the cause, severity, and extent of the damage. Early intervention and consistent rehabilitation efforts are key to improving outcomes and helping individuals regain their independence.
If you or a loved one is facing the challenges of cerebellum brain damage, you don’t have to go through it alone. At NueLife Rehabilitation, we specialize in personalized, evidence-based neuro rehabilitation, including TBI rehabilitation and stroke patient rehab programs designed to restore function, improve mobility, and enhance quality of life.
Want to learn more about the different types of brain damage and how we can help? Explore our blogs on:
Get expert support, compassionate care, and real results. Contact us today to learn how our team can guide you on your path to recovery.
***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Recovering from a brain injury can be a long process. Patients go through various stages of rehabilitation and recovery. Patients who can transition through each stage increase the likelihood of healing, aiming to move the patient as close as possible to their pre-injury condition.
Generally, there may be ten stages that a patient with a traumatic brain injury (TBI) may experience or progress through. However, not every person will experience each stage in identical ways, and each survivor will recover at a different pace.
This blog post will walk you through the 10 stages of TBI recovery based on the Rancho Los Amigos Levels of Cognitive Functioning and highlight techniques to promote optimal healing.
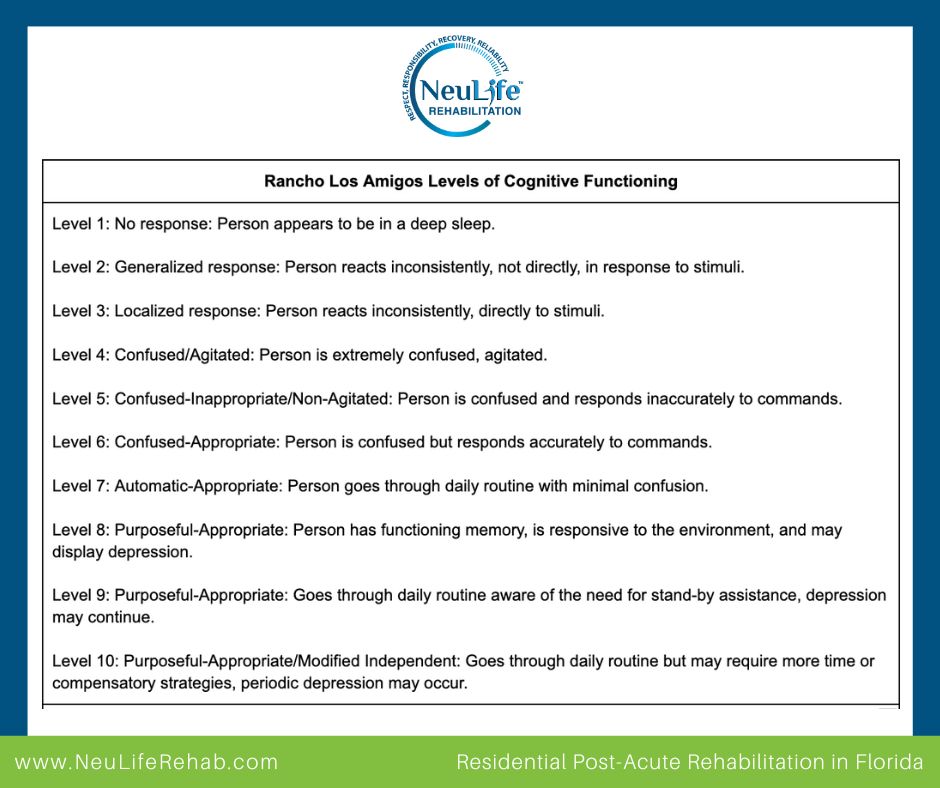
The Rancho Los Amigos Scale was developed at the Rancho Los Amigos National Rehabilitation Center in California. It is a widely used clinical tool that describes the cognitive and behavioral patterns of TBI patients during recovery.
The scale consists of 10 levels, ranging from complete unresponsiveness to the ability to function independently. Understanding these stages helps medical professionals, caregivers, and families set realistic expectations and provide appropriate support.
A coma is the deepest state of unconsciousness. It allows the brain to heal uninterrupted. With a severe injury, the patient may remain in a coma for some time. This is considered the first stage of TBI recovery.
What to expect:
Generally, coma patients have no eye movement, no purposeful movement, and lack speech and communication. The patient is unresponsive to the environment and does not wake, even with stimulation.
Comas can last weeks, months, or even years. After awakening from a coma, the patient may move through further stages of recovery.
Care approach:
Comas and a vegetative state are not the same; they are different states of consciousness. Neurological responses differ between these two. Patients in a coma have no neurological response, while those in a vegetative state may have regained some reflexes.
What to expect:
In a vegetative state, the patient may appear awake. You may see eye movement, reaction to stimulation, and involuntary body movements. These movements are caused by responses in the brain that remain intact after injury and because areas of the brain have begun to heal.
Care approach:
Once patients react and can communicate, they move to the next stage of recovery.
During this stage, patients may come in and out of consciousness. The significant improvement seen is awareness of people and surroundings. When in this stage, medications can help stimulate the brain to regain consciousness.
What to expect:
The patient responds more deliberately to specific stimuli, such as turning their head toward a voice or following simple commands. They begin to recognize familiar faces and have more purposeful movements.
Care approach:
As the patient responds to instructions and communication, they move toward recovery.
Post-traumatic amnesia is the stage after the patient emerges from a coma. They may experience a state of amnesia upon awakening. There are two types of amnesia:
What to expect:
Some patients may show behavior changes in this stage. They may become highly confused and aggressive or show other signs of inappropriate behavior. Patients can also lose their sense of inhibition, especially if the frontal lobe experiences an injury.
They may also experience difficulties processing information and not recognizing their surroundings.
Care approach:
Once patients can consistently remember daily events and amnesia diminishes, they are usually ready to begin rehabilitation at a neuro rehab facility, where true healing and recovery begin.
In this stage, patients can have difficulty focusing on tasks and may be confused. It can be challenging for them to respond during communication or express inaccurate or unintelligible communication.
What to expect:
During this stage, their short-term memory is still impaired, so expect them to experience difficulties in communication and learning new information. They may also do random speech with little awareness of conversation.
Care approach:
If you want to learn more about inappropriate behavior after TBI, check out our blog post on brain injury and inappropriate behavior.
During this stage, the patient may be able to communicate and follow more commands from staff. However, memory issues often still exist, and focusing on tasks can be challenging.
What to expect:
Expect patients to have better attention spans but still be forgetful. With help, they can now engage in familiar activities.
Care approach:
When patients advance to this stage in their recovery, they can begin to follow a schedule and complete some daily life activities independently.
This is an essential stage in post-acute rehabilitation, as patients can participate in important rehab recovery efforts, including physical therapy, occupational therapy, and speech therapy.
What to expect:
Patients may have improved memory for familiar tasks but struggle with problem-solving, decision-making, and planning skills.
Care approach:
At this stage, the patient's awareness and memory have improved. However, the patient may continue to struggle with social interaction, reaction time, and handling unexpected situations that are not part of their routine.
That said, they often have made significant improvements in their coping skills and may sometimes be able to graduate from a rehabilitation facility and return home.
Care approach:
The TBI patient has gained function in this stage and can perform most tasks independently. They likely will need to have continued rehabilitation for brain injury but do not require the full assistance of a neurorehabilitation center.
What to expect:
Patients in this stage can manage appropriate activities independently but may need assistance in complex or unfamiliar situations. Furthermore, they have improved emotional stability and can make decisions with occasional support.
Care approach:
During this final stage, some patients have a full recovery and can handle daily life activities on their own. However, their cognition may remain slower than pre-injury, which they usually do well with, and they can participate in outpatient neuro services if necessary.
Care approach:
Maximizing recovery potential requires a combination of medical, cognitive, and emotional support. Here are some key techniques:
Neulife Rehab is one of Florida's most extensive brain injury facilities in the southwest United States. Neulife is CARF-accredited (Commission on the Accreditation of Rehabilitation Facilities) in Brain Injury Specialty Programs and Residential Rehabilitation.

Through rehabilitation, medical management, psychiatric, neurophysical services, occupational, speech, and cognitive therapies, and much more. We provide different types of programs, from traumatic brain injury rehabilitation to stroke patient rehab. We provide the best in care so your loved one has the BEST POSSIBLE recovery.
Schedule a tour to see our facility and decide if it may be appropriate for your loved one. We are always here to answer questions. Please reach out to us at 1-888-626-3876.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
The human brain is a complex and intricate organ responsible for countless functions, including movement, emotion, and perception. One of its most crucial parts is the occipital lobe, which is located at the back of the head and is responsible for visual processing and perception. Any damage to this area can significantly impact a person's ability to see and understand the world around them.
This blog will discuss the symptoms of occipital lobe damage, its causes, and potential treatment options. Whether you are a medical professional, a caregiver, or someone looking to educate themselves, this comprehensive guide will equip you with the knowledge to recognize and manage the symptoms of occipital lobe damage and access top-quality neuro rehabilitation.
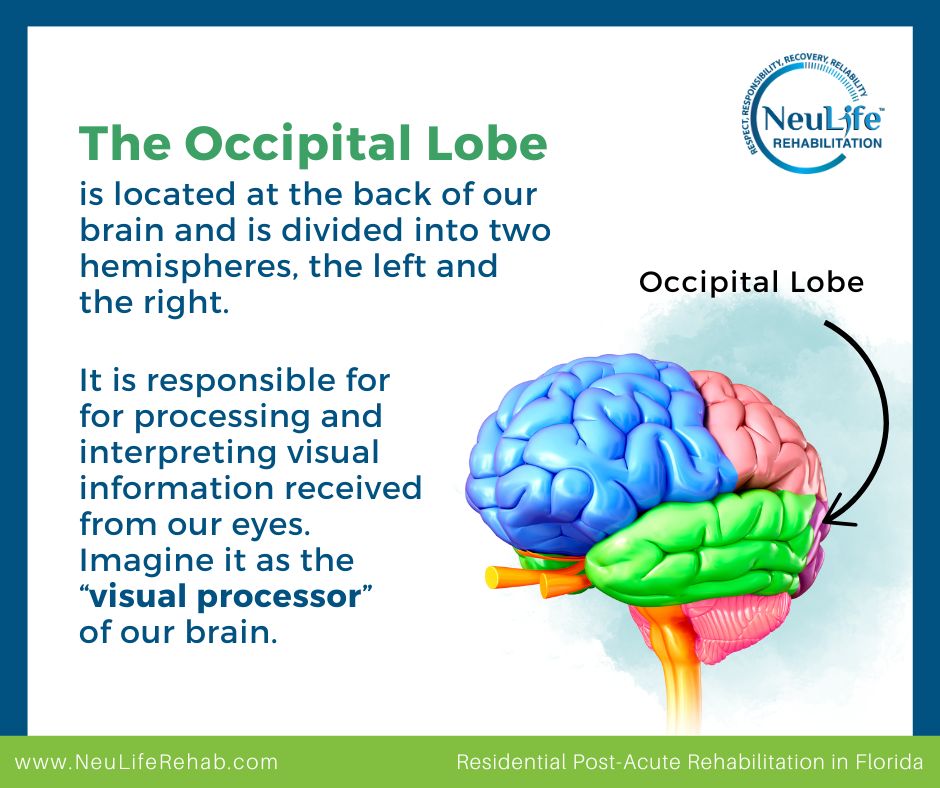
The occipital lobe is one of four lobes that make up the cerebral cortex, the outer layer of our brain. It is located at the back of our brain and is divided into two hemispheres, the left and the right.
The occipital lobe is responsible for processing and interpreting visual information received from our eyes. It takes in information such as color, shape, and motion and then translates it into meaningful images that we can see. Imagine it as the “visual processor” of our brain.
Occipital lobe damage can result from various factors, including:
This can occur due to a severe blow or jolt to the head, which damages brain tissue.
When blood flow to the occipital lobe is disrupted, it can result in brain damage.
A weakened blood vessel in the brain can burst, causing bleeding in the occipital lobe and causing damage.
A tumor in or near the occipital lobe can press against the brain tissue, causing damage.
Certain infections, such as meningitis, encephalitis, or abscesses, can cause inflammation and damage the occipital lobe.
Aside from the effects on vision, occipital lobe damage can also cause other neurological symptoms, depending on the location and extent of the damage. These symptoms may include:
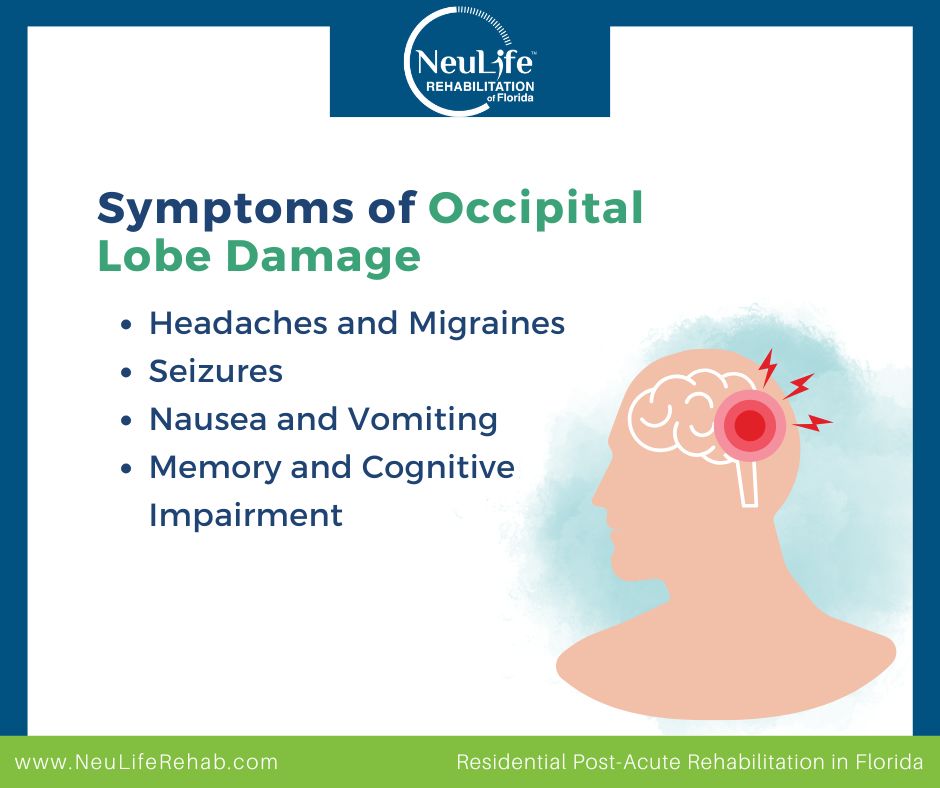
Damage to the occipital lobe can cause persistent headaches and migraines, particularly in the back of the head.
The occipital lobe is closely linked to the temporal lobe, responsible for processing emotions. Damage to the occipital lobe can trigger seizures in the temporal lobe, leading to mood, behavior, or consciousness changes.
Occipital lobe damage can also cause nausea and vomiting, similar to the symptoms experienced during a migraine.
The occipital lobe integrates visual information with other sensory inputs, so damage to this area can cause memory and cognitive impairment. This could also include difficulty with spatial awareness, motor coordination, and language processing.
The effects of occipital lobe damage on vision can vary, depending on the extent and location of the damage. For instance, damage to the left occipital lobe can cause issues with the right visual field and vice versa.
Some of the common effects of occipital lobe damage on vision include:
The most common effect of occipital lobe damage is visual impairment. This can range from mild vision loss, such as blurred or double vision, to complete blindness in one or both eyes.
Damage to the occipital lobe can result in blind spots or scotomas in the visual field. This means the individual may have difficulty seeing objects in certain parts of their visual field. For example, damage to the right occipital lobe may result in a blind spot in the left visual field.
The occipital lobe plays a crucial role in object recognition. Damage to this area can make recognizing familiar objects, faces, or surroundings difficult, a condition known as visual agnosia.
The occipital lobe also helps us see colors and distinguish between them. Damage to this region can result in difficulties with color perception, leading to color blindness.
Occasionally, occipital lobe damage can result in visual hallucinations, where an individual sees objects or patterns that are not present. This is known as Charles Bonnet Syndrome and is more common in older adults.
The recovery process for occipital lobe damage is complex and varies depending on the severity and cause of the injury. However, with proper diagnosis and treatment, individuals can experience significant improvements in their vision. Here are the steps involved in the recovery process:
The first step in the recovery process is to seek medical attention immediately after the occipital lobe damage is detected. A neurologist or eye specialist will conduct a series of tests to assess the extent of the injury and determine the best course of treatment.
Vision therapy is a specialized form of TBI rehabilitation focusing on improving visual function and processing. It typically involves a combination of eye exercises and activities to strengthen and retrain the brain's visual pathways.
Along with vision therapy, occupational therapy can help individuals with occipital lobe damage regain independence and improve their daily living skills. This may include techniques to compensate for visual field loss, such as using aids like magnifiers and filters.
As occipital lobe damage can lead to emotional distress, incorporating cognitive-behavioral therapy can help individuals cope with the changes in their vision and adjust to their new normal.
A healthy lifestyle, including a balanced diet, regular exercise, and adequate rest, is essential for recovery. These habits can help optimize brain and eye function and speed up healing.
At NeuLife Rehabilitation, a top-tier post acute rehabilitation center, we are committed to helping individuals with occipital lobe damage regain their independence and thrive. With our personalized approach, we offer the best possible care and support for our patients on their journey to recovery.
If you or a loved one has suffered from occipital lobe damage and is looking for a stroke patient rehab, do not hesitate to contact us. Our experienced team is here to guide you through the recovery process and provide the best possible care. Along with our exceptional care, we also offer informative blogs on a variety of topics, including
Contact us today to begin your journey towards a brighter future. Let us be your trusted partner in achieving optimal recovery.

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
After a traumatic brain injury (TBI), many individuals experience heightened sensitivity to sensory input—a condition known as sensory overload or overstimulation.
Everyday sights, sounds, smells, and even social interactions can become overwhelming and may trigger intense discomfort and distress. This can make daily life challenging, leading to fatigue, anxiety, and difficulty concentrating.
Sensory overload occurs when the brain struggles to process and filter sensory information. After a TBI, the brain’s ability to regulate sensory input is often disrupted. Some common causes of sensory overstimulation in brain injury patients include:
Sensory overload manifests in different ways for each person, but common symptoms include:
Managing sensory overload requires a combination of environmental modifications, self-regulation techniques, and coping strategies. Here are some helpful practices you can do:
When sensory overload strikes, having immediate strategies to employ can provide rapid relief and prevent the escalation of symptoms.
Making thoughtful modifications to your living and working environments can significantly reduce the frequency and intensity of sensory overload episodes. Some examples include:
Incorporating relaxation techniques into your daily routine is crucial for long-term management of overstimulation. These techniques help regulate the nervous system and build resilience to sensory triggers over time.
Some examples of relaxation techniques include mindfulness meditation, progressive muscle relaxation, and deep breathing exercises.
Occupational therapists can provide personalized strategies for managing sensory challenges. Counseling or cognitive-behavioral therapy (CBT) can also help with emotional responses to overstimulation.
A sensory diet is a structured plan of sensory activities that help regulate the brain’s response to stimuli. Think of it as creating a balanced “sensory meal” for your brain throughout the day, ensuring it receives the right types and amounts of sensory input to function optimally.
Occupational therapists often design sensory diets to match an individual’s needs. Here are some common sensory diet activities for managing overstimulation:
While managing sensory overload can be challenging, long-term improvement is possible with patience and the right strategies. Here are key steps for overcoming sensory overload after a brain injury:
Keep a journal to track which environments, sounds, or activities cause overstimulation. This can help you make necessary adjustments to avoid triggers.
Instead of avoiding all sensory input, slowly increase exposure in a controlled way to help the brain adapt.
Quality sleep and a healthy diet can enhance brain function and resilience, making sensory overload less intense.
Helping loved ones understand overstimulation can lead to more supportive environments and interactions.
Recovery takes time. Setting small, achievable goals can help track progress and build confidence.
Professional support is invaluable in navigating the complexities of overstimulation after a brain injury. It’s important to work with healthcare professionals who can help you overcome the different challenges that come with this condition.
At NeuLife Rehabilitation, we understand that recovering from a TBI involves more than just healing from the initial trauma. Many individuals also struggle with challenges like sensory overstimulation, cognitive difficulties, and emotional changes. That’s why our comprehensive neuro rehab program is designed to not only treat TBI but also help patients overcome the conditions that often come with it.

As a leading post-acute rehabilitation center, we provide individualized care plans that support stroke patient rehab, orthopedic recovery, and neurological conditions. Our expert team is committed to helping patients regain independence and improve their quality of life.
Contact our traumatic brain injury rehabilitation center to learn more.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Patients with TBI often face cognitive, physical, and emotional hurdles as they work to regain their independence and quality of life.
Fortunately, games designed to stimulate the brain can play a pivotal role in their recovery process. Not only do these games help patients rebuild critical cognitive functions, but they also provide a sense of accomplishment and fun.
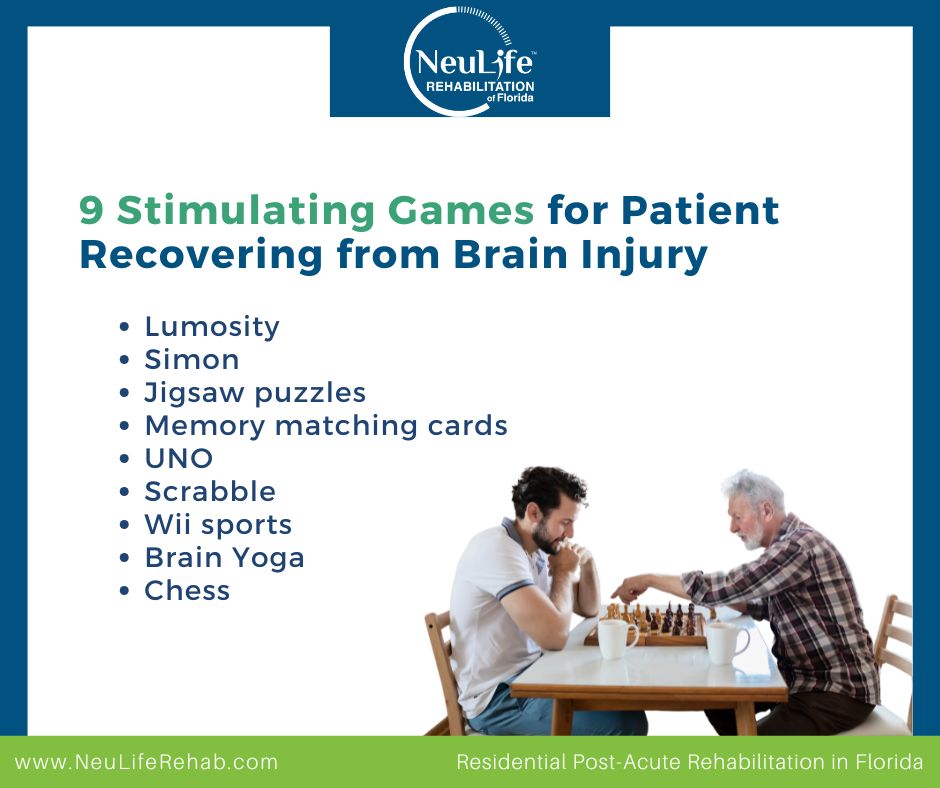
Read on below to learn about nine engaging games that are ideal for enhancing brain injury recovery.
Games offer a unique and enjoyable way to stimulate the brain while addressing deficits caused by injury. Cognitive rehabilitation often requires repetitive practice, which can sometimes feel monotonous. Games provide a more engaging alternative by incorporating strategy, problem-solving, and memory exercises into entertaining formats.
By playing games, patients can target various cognitive functions, including:
Games also create opportunities for social interaction, reducing feelings of isolation and promoting emotional well-being. Overall, incorporating games into recovery plans can make rehabilitation more dynamic and effective.
Not all games are equally beneficial for brain injury recovery. When selecting games, it is essential to consider the following features:
Selecting games that meet these criteria ensures they will be both enjoyable and effective for rehabilitation.
Lumosity is an online platform offering a wide variety of brain-training games. These games target cognitive skills like memory, attention, and problem-solving through engaging timed challenges.
How it helps: Each game adapts to the user’s performance, ensuring a personalized experience that grows with their abilities. This progressive difficulty is excellent for brain injury patients, as it helps them steadily rebuild skills without feeling frustrated.
How to play: Patients can play Lumosity on a computer or mobile device. An example is “Speed Match,” where players quickly identify whether shapes match. Therapists can adjust session lengths or specific games to align with therapy goals.
Simon is a classic memory game that involves replicating increasingly complex patterns of lights and sounds. It’s simple yet highly effective for cognitive stimulation.
How it helps: This game targets short-term memory, attention, and pattern recognition, essential areas for brain injury recovery.
How to play: Players follow a sequence of flashing lights and sounds, repeating them in the same order. To adapt, caregivers can start with shorter sequences or provide verbal cues if needed.
Jigsaw puzzles involve assembling interlocking pieces to create a complete image. They come in various difficulty levels, making them accessible for all patients.
How it helps: Puzzles improve problem-solving skills, spatial awareness, and fine motor coordination, all crucial for brain recovery.
How to use: Start with puzzles containing fewer pieces and gradually increase the complexity as the patient progresses. Adaptive puzzles with larger or textured pieces are ideal for those with limited dexterity.
Memory matching games involve flipping over cards to find matching pairs. It’s simple, yet it provides a powerful cognitive workout.
How it helps: This game strengthens short-term memory, attention, and visual recognition.
How to play: Use decks with familiar themes or images (e.g., animals or shapes). Start with fewer pairs and increase the number as the patient’s memory improves. Caregivers can also assist by giving verbal prompts.
UNO is a popular card game where players match cards by color or number, aiming to be the first to discard all their cards.
How it helps: This game enhances color and number recognition, memory, and strategic thinking, all while promoting social interaction.
How to play: Players take turns matching a card from their hand to the one on the discard pile. The game can be adapted for brain injury patients by simplifying the rules, playing with fewer cards, or providing hints to encourage participation and confidence.
Scrabble is a word game where players create words on a board using letter tiles. It combines vocabulary skills with strategic thinking.
How it helps: This game enhances language processing, memory, and critical thinking, especially for patients recovering from language-related impairments.
How to play: To adapt Scrabble for brain injury patients, use a simplified version with fewer tiles or allow more time to form words. Playing in teams can also reduce pressure and make it more social.
Wii Sports is a motion-based video game that simulates activities like tennis, bowling, and golf.
How it helps: The game combines physical movement with cognitive coordination, making it excellent for patients working on both motor and cognitive rehabilitation.
How to play: Patients use motion-sensing controllers to play virtual sports. Therapists can select low-impact games like bowling to suit the patient’s physical abilities.
Brain Yoga is a mobile app that combines relaxation with cognitive challenges like puzzles, word searches, and math exercises.
How it helps: It targets multiple cognitive skills, including memory, logic, and attention, while promoting stress relief.
How to play: Patients can select specific games based on their rehabilitation goals. For example, a word search can enhance language processing, while math puzzles improve problem-solving.
Chess is a strategy game that requires players to plan moves, anticipate the opponent’s actions, and think several steps ahead.
How it helps: This game enhances problem-solving, strategic thinking, and concentration, making it ideal for brain injury recovery.
How to play: Start with simplified rules or focus on a few pieces to reduce complexity. Caregivers or therapists can guide patients through the thought process behind each move to build confidence.
NeuLife Rehabilitation provides a state-of-the-art, holistic approach to brain injury recovery, offering 24/7 care and personalized therapies tailored to each patient’s needs.

We provide the following services:
Our programs integrate cognitive and physical rehabilitation techniques, including the use of stimulating games and activities to enhance recovery.
With a dedicated team of experts and a supportive environment, NeuLife empowers patients to regain independence and improve their quality of life.
Contact us today and discover how we can help you or your loved one thrive after a brain injury!
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
The temporal lobe, located in the brain's cerebral cortex, plays a crucial role in memory, language, emotion, and some aspects of hearing and vision. Damage to this vital area can have significant and lasting effects on an individual's cognitive and emotional functioning.
Whether from a traumatic brain injury, stroke, or other medical condition, understanding how temporal lobe damage can impact a person's life is paramount to providing effective treatment and supporting their recovery.
In this blog, we will dive into the causes and symptoms of temporal lobe damage, explore various treatment options, and discuss the recovery process. Moreover, we will also discuss how NeuLife Rehabilitation of Florida can help those suffering from temporal lobe damage to regain control of their lives.
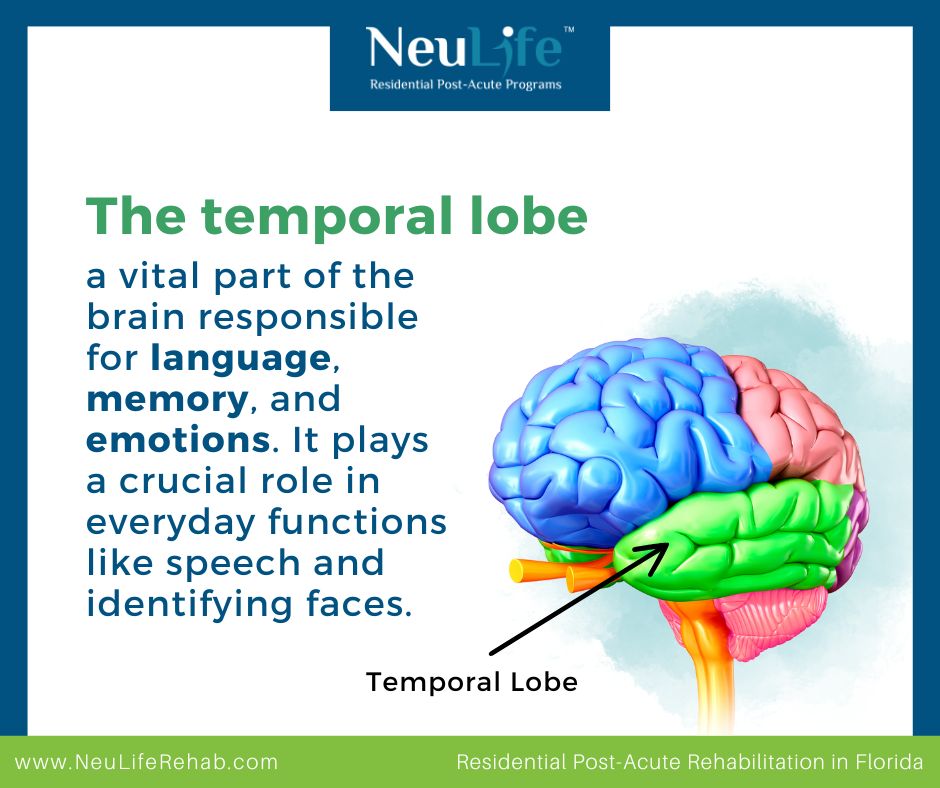
The temporal lobe is located on the side of the brain, just behind the ears. It is one of the four cerebral cortex lobes, along with the frontal, parietal, and occipital lobes. The primary function of the temporal lobe includes:
The temporal lobe processes auditory information, including sound recognition and speech perception. It contains the primary auditory cortex, which receives signals from the ears and interprets them as meaningful sounds. This information then travels to other brain parts for further processing, allowing us to understand and respond to what we hear.
The temporal lobe also plays a critical role in language processing. It is responsible for understanding and producing spoken language. The left temporal lobe, in particular, is involved in speech production, while the right temporal lobe is responsible for understanding the emotions conveyed through speech.
The temporal lobe is closely connected to the hippocampus, a structure located deep in the temporal lobe responsible for forming and storing memories. Together, they play a crucial role in consolidating and retrieving long-term memories. This brain region is also responsible for recognition memory, which helps us identify objects, people, and places based on previous experiences.
The temporal lobe also plays a role in regulating our emotions. The amygdala, a small structure located within the temporal lobe, is responsible for processing and responding to emotional stimuli. It helps us recognize and respond appropriately to emotions such as fear, pleasure, and anger.
Temporal lobe damage can have a significant impact on a person's life. The effects can vary depending on the extent and location of the damage. Some common effects include:
The temporal lobe plays a crucial role in memory formation and retention. Therefore, damage to this area can lead to memory loss, making it difficult to recall past events and retain new information.
As mentioned earlier, the temporal lobe is responsible for processing auditory information. Damage to this area can cause difficulties in understanding and interpreting speech, making it hard for a person to communicate effectively.
Vision is also controlled by the temporal lobe, specifically the occipitotemporal cortex. Damage to this area can result in visual disturbances, such as difficulty recognizing faces or objects.
The temporal lobe is connected to the limbic system, the part of the brain responsible for regulating emotions and behavior. Damage to this area can lead to mood, personality, and behavior changes.
Damage to the temporal lobe can also cause sensory disturbances, such as changes in the perception of touch, smell, and taste. This can significantly affect a person's daily life, making it difficult to perform basic tasks.
The treatment for temporal lobe damage depends on the underlying cause and the severity of the damage. Some common treatments include:
Medications, such as anticonvulsants and antidepressants, may be prescribed to manage seizures and mood changes associated with temporal lobe damage. These medications help to control symptoms and improve the quality of life for those with this condition.
In some cases, surgery may be recommended to remove the damaged part of the temporal lobe. This can help reduce seizures and improve symptoms in individuals with severe temporal lobe damage.
Psychotherapy, such as cognitive-behavioral therapy, can help individuals with temporal lobe damage cope with changes in behavior and emotions. It can also assist in managing memory and communication difficulties.
Rehabilitation programs, such as those offered at NeuLife Rehabilitation of Florida, can help individuals with temporal lobe damage regain their independence and improve their quality of life. These programs focus on maximizing functioning and adapting to new ways of performing daily tasks.
The recovery process for temporal lobe damage can vary from person to person, depending on the severity of the damage and the treatments they receive. In some cases, individuals may experience a full recovery, while others may require ongoing therapy and support.
The recovery process may involve:
Physical rehabilitation can help individuals with sensory and motor difficulties caused by temporal lobe damage. It includes exercises and therapies to improve strength, coordination, and balance.
Occupational therapy can assist individuals in relearning daily tasks and adapting to any physical or cognitive impairments caused by temporal lobe damage. It aims to improve functional skills and promote independence.
Speech therapy can help individuals with communication difficulties caused by temporal lobe damage. It focuses on improving speech, language, and swallowing abilities.
Coping with the effects of temporal lobe damage can be emotionally challenging. Therefore, emotional support from family, friends, or a professional therapist can significantly aid recovery.
If you or a loved one is struggling with temporal lobe damage, rest assured that you are not alone in this journey. At NeuLife Rehabilitation in Florida, we recognize the challenges and difficulties associated with this condition.
Our neuro rehabilitation services are designed to cater to the unique needs of each individual, helping them regain their independence and enhance their overall well-being. Our post-acute rehabilitation center has successfully aided numerous patients with temporal lobe damage in their recovery.
Our team of experienced healthcare professionals, including physicians, therapists, and nurses, is committed to providing exceptional care and support to our patients. We invite you to schedule a tour and visit our facility to see how our services can benefit you or your loved one on the road to healing.
Interested in learning more about brain injury and recovery? Check out our latest blogs on "What Parts of the Brain are Affected by TBI?" and "Frontal Lobe Functions: What to Expect and How to Recover." Our experienced team is dedicated to providing valuable resources and information to those affected by temporal lobe damage.
At NeuLife, we also specialize in TBI rehabilitation, stroke patient rehab, and other brain injury treatments. Let us be a part of your healing journey. Contact us to learn more about our services and how we can assist you or your loved one recover from temporal lobe damage.

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
The frontal lobes are a crucial part of our brain that plays a significant role in our behavior, thoughts, and emotions. They regulate our decision-making, problem-solving, planning, and other critical cognitive functions. But what happens when these frontal lobes are damaged or impaired? How does it affect our daily life, and what can be done to recover from it?
In this blog post, we will explore the functions of the frontal lobes, what to expect when they are damaged, and how NeuLife Rehabilitation of Florida can help recover through neuro rehabilitation.
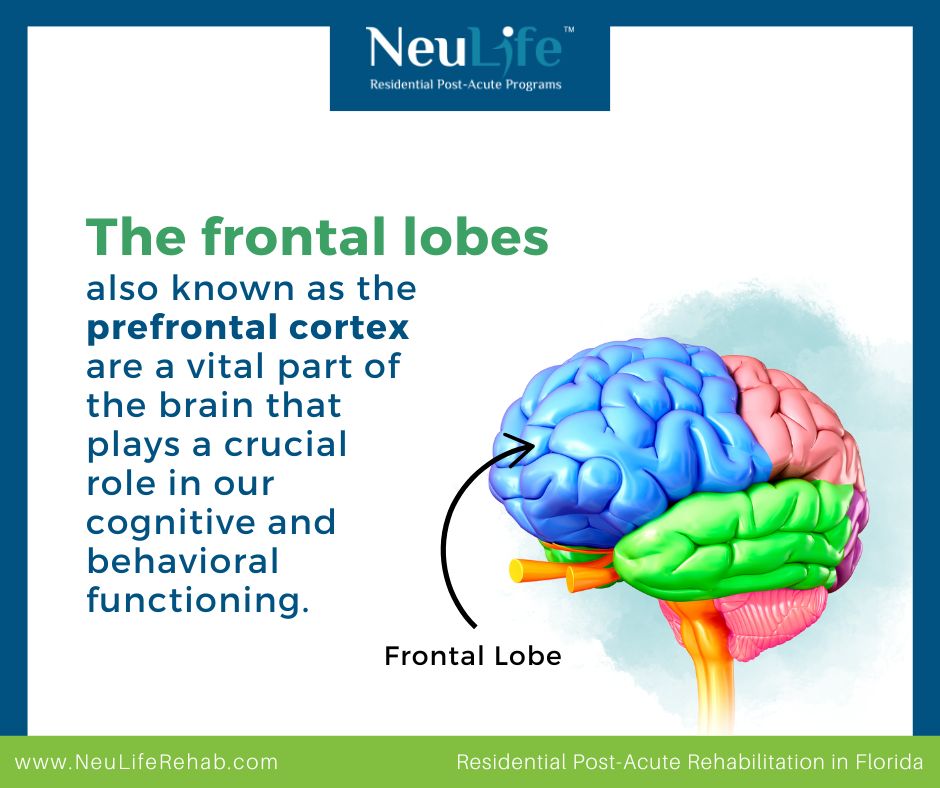
The frontal lobes, also known as the prefrontal cortex, are a vital part of the brain that plays a crucial role in our cognitive and behavioral functioning. Located in the front of the brain, just behind the forehead, the frontal lobes are responsible for various functions essential to our daily lives, including:
Frontal lobe injuries can result from a variety of causes, including traumatic brain injuries, strokes, and tumors. These injuries can significantly impact a person’s life, affecting cognitive, emotional, and physical functioning.
Some common symptoms of frontal lobe injuries include:
Due to the critical role the frontal lobes play in regulating emotions, an injury to this brain area may result in personality changes. This can manifest as increased aggression, irritability, and impulsivity.
As mentioned earlier, the frontal lobes are involved in decision-making and problem-solving. When injured, a person may have difficulty making simple decisions or planning steps to reach a goal.
Depending on the severity and location of the injury, a person may experience motor deficits, such as weakness or paralysis on one side of the body, difficulty with coordination and balance, and changes in fine motor skills.
Frontal lobe injuries can also affect a person’s ability to speak and understand language. They may have trouble finding the right words, forming sentences, or understanding what others are saying.
Injuries to the frontal lobes can also impact a person’s memory, making it difficult to remember recent events or learn new information.
Recovering from a frontal lobe injury can be a long and challenging process, but with the proper support and rehabilitation, it is possible.

At NeuLife Rehabilitation of Florida, we understand the complex nature of frontal lobe injuries and the impact they can have on a person’s life. Our team of experienced and compassionate professionals uses a comprehensive, person-centered approach to help individuals recover from their injuries and regain their independence.
Some of the therapies and programs we offer for frontal lobe injury recovery include:
Our occupational therapists work with individuals to improve their daily living skills, such as dressing, grooming, and meal preparation, which may be affected by a frontal lobe injury.
Our physical therapists help individuals improve their strength, balance, and coordination through exercise and other techniques.
Our speech therapists work with individuals to improve their speech and language abilities, including expressive and receptive language skills.
Our cognitive therapists use various techniques to address deficits in memory, problem-solving, and other mental functions affected by a frontal lobe injury.
This type of counseling provides a safe and supportive environment to address and overcome the psychological effects of frontal lobe injuries, leading to improved overall well-being and quality of life.
As we age, taking care of this vital part of our brain is essential to ensure its proper function. Here are some tips for maintaining a healthy frontal lobe.
If you or someone you know has experienced frontal lobe damage, do not lose hope. Recovery is possible, and NeuLife Rehabilitation of Florida can help. Neulife Rehab is one of the largest residential post-acute rehabilitation centers in the southeast specializing in TBI rehabilitation, stroke patient rehab, SCI, Complex Ortho & Neurological Disorders rehabilitation.
Our programs are accredited by the Commission on Accreditation of Rehabilitation, and our experienced and dedicated professionals are committed to providing the best care and support for our client's recovery journey.
To educate and support individuals with frontal lobe damage, we have written a blog titled "What Parts of the Brain are Affected by TBI?" Join us on this journey towards a better tomorrow and schedule a tour of our facility today.
***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Traumatic Brain Injury (TBI) can make it hard to speak, understand language, or even remember things. Speech therapy helps TBI survivors recover their communication skills. In this blog post, we’ll find and learn the best speech therapy activities for TBI survivors that help with aphasia, apraxia, and other speech challenges.
A brain injury can affect different brain parts, making speaking or understanding language difficult. TBI survivors may have trouble finding the right words, forming sentences, or pronouncing sounds clearly, often due to damage in areas of the brain that control language and speech muscles.
Everyday speech challenges after a TBI include aphasia, which affects understanding or using words; apraxia, which makes pronouncing words or sounds difficult; and dysarthria, which causes weakness in the muscles needed for speaking.
What is Aphasia? Aphasia is a language disorder caused by damage to the brain’s language centers. People with aphasia may have trouble speaking, understanding words, reading, or writing. It can be frustrating because the person knows what they want to say but can’t find the right words.
These are example therapy exercises for Aphasia.
Using word puzzles or apps helps improve vocabulary and word recall. These activities challenge the brain to remember words and their meanings. Word searches or crossword puzzles also encourage word retrieval, making it easier to recall words in everyday conversation.
Practice putting words together to form sentences. Start with simple sentences and work toward more complex ones. By practicing how words fit together, individuals with aphasia can become more confident in communicating in sentences rather than just isolated words.
Reading out loud helps improve word recognition and speech fluency. It’s also a great way to practice pronunciation and sentence structure. Repeating reading aloud supports the connection between written and spoken words, improving overall language comprehension.
Use pictures or photos and describe what’s happening in them. This helps with word recall, organizing thoughts, and forming meaningful sentences. It also strengthens the ability to articulate ideas effectively, improving spoken and written language.
Speech therapy activities help TBI survivors improve these skills, regain confidence, and communicate more easily.
A critical part of speech recovery after a TBI is strengthening your facial and mouth muscles. These muscles help you talk, chew, and swallow. If they become weak, it can make speaking harder. To help with this, several facial strengthening activities can improve muscle strength and coordination.
Incorporating these simple activities into a daily routine can help TBI survivors regain their speech clarity and muscle strength over time.
What is Apraxia? Apraxia is a motor speech disorder that makes coordinating the muscles needed for speaking hard. This means that even if the brain knows what to say, the mouth has trouble moving in the right way to say it. Apraxia after a TBI is common and can cause slurred speech or difficulty pronouncing words. Speech therapy activities can be very useful in helping with apraxia.
Repeating simple sounds or syllables like "ba," "pa," or "ma" helps retrain the brain and mouth muscles to produce speech more clearly. This strengthens speech production and muscle coordination over time.
Encouraging slow, deliberate speech helps with pronunciation and gives the brain more time to organize words and form clear sentences. This approach improves speech clarity by focusing on how each word is spoken.
Practicing tongue, lips, and jaw movements through exercises like saying "pa-ta-ka" can improve muscle coordination and rebuild motor control for more explicit speech. These exercises should be done slowly and carefully to reinforce proper muscle use.
Visual aids (like pictures) or tactile cues (such as gently guiding the jaw or mouth) can help remind the brain how to form specific sounds. These cues ensure the correct muscle movements are made when pronouncing certain words.
Through consistent practice and speech therapy, individuals with apraxia can improve their speech clarity, motor control, and confidence in communication.

Consistency and practice are essential to get the most out of speech therapy. Here are a few tips for maximizing the benefits of speech therapy activities:
Regular practice can lead to noticeable speech and language improvement, even for just a few minutes each day. The more you practice, the more progress you can make.
Recovery from TBI takes time, so it’s essential to stay patient and persistent. Celebrate small victories and focus on gradual improvement rather than expecting quick results.
A speech therapist can provide personalized guidance tailored to specific speech challenges. They can track progress, suggest helpful exercises, and give feedback on how to improve speech skills.
Practicing speech therapy activities with loved ones can provide additional support and motivation and make the process more enjoyable and rewarding.
Many apps and online tools are designed to make speech practice fun and interactive. These tools can be used at home or on the go to reinforce learning and provide extra practice outside therapy sessions.
Speech therapy plays a crucial role in the recovery process for TBI survivors. By practicing activities that target specific challenges like aphasia, apraxia, and muscle weakness, individuals can regain their ability to communicate more clearly and confidently. With time, patience, and consistent effort, TBI survivors can rebuild their speech and improve their quality of life.
If you or someone you care about is recovering from a brain injury, speech therapy can make a big difference. NeuLife Rehabilitation in Florida offers some of the best speech therapy activities to help TBI survivors speak and understand better and boost their confidence.
Whether you're looking for a neuro rehabilitation center or need support with post-acute rehabilitation, our expert team is ready to guide you through every step of recovery. Our TBI rehabilitation centers are designed to provide the best care and help you make real progress.
Don’t wait! Begin the journey to recovery today! Discover NeuLife Rehabilitation’s comprehensive programs designed specifically for TBI patients, including speech therapy activities to improve communication, memory, and overall cognitive function. Take the first step toward a better quality of life now!
Want to Visit NeuLife Rehabilitation? Schedule a tour NOW

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
According to the Centers for Disease Control and Prevention (CDC), more than 38 million Americans have diabetes, and 1 in 5 of them do not know they have it. People with diabetes have an increased risk of developing other health conditions, such as heart disease, blindness, and kidney disease.
In this blog, we will dive deeper into the connection between diabetes and brain injury, exploring the causes, symptoms, and potential treatment options. So, let’s explore this topic further and discover what the research has to say about the complex relationship between these two conditions.
Diabetes is a chronic condition that occurs when the body is unable to produce or effectively use insulin, a hormone responsible for regulating blood sugar levels. This results in high blood sugar levels, which can cause damage to various organs and systems in the body.
There are two types of diabetes – type 1 and type 2.

Type 2 diabetes can develop slowly, and some individuals may not experience any symptoms in the early stages. However, as the disease progresses, they may start to notice the following signs:
There is a strong link between diabetes and brain injury. In fact, people with diabetes are more likely to experience brain damage compared to those without diabetes.
Diabetes can lead to damage in the small blood vessels in the brain. These blood vessels are responsible for supplying oxygen and important nutrients to the brain cells. When these vessels get damaged, it can result in a stroke, which is a medical emergency that occurs when blood flow to the brain gets blocked. This lack of oxygen and nutrients can cause brain cells to die, leading to permanent brain damage.
Apart from strokes, diabetes can also increase the risk of developing dementia, a group of conditions that affect the brain and cause a decline in memory, thinking, and behavior. Research has shown that diabetes can accelerate the progression of Alzheimer's disease, a type of dementia, by causing damage to brain cells.
But can diabetes also affect the brain? The answer is yes. Diabetes can potentially lead to brain injury or worsen its effects, making treatment more challenging.
One of the most common effects of diabetes on the brain is nerve damage, also called diabetic neuropathy. This condition affects the nerves in the arms, legs, and feet, causing pain, numbness, and tingling sensations. These symptoms can affect balance and coordination, increasing the risk of falls and accidents, leading to brain injury. Moreover, diabetic neuropathy can also affect the autonomic nervous system, which controls bodily functions such as blood pressure and heart rate. This can affect the body's response to brain injury, making it difficult to detect and treat.
Diabetes can also impact the treatment of brain injury in other ways. People with diabetes often have weaker immune systems, making them more susceptible to infections. This can increase the risk of infection following a brain injury. Furthermore, diabetes can also affect the body's ability to heal, thus prolonging the recovery process. It can also interfere with the effectiveness of medication used to treat brain injury, potentially worsening the condition.
The good news is that there are steps you can take to protect your brain if you have diabetes. Here are some steps you can take to keep your blood sugar levels under control:
Failing to recognize the potential effects of diabetes and brain injury can have detrimental, lasting effects on your well-being and recovery. At NeuLife Rehabilitation, we are well aware of the complexities involved in managing both conditions simultaneously. Our personalized rehabilitation for brain injury and treatment plans are specifically tailored to address this unique combination.
Don't hesitate any longer - take charge of your health and place your trust in our highly skilled team to guide you towards optimal recovery. Don't allow the correlation between diabetes and brain injury to hinder your progress any further. It's time to take the first step towards a brighter and healthier future with our expert neuro rehab and post acute rehabilitation services for brain injury.
***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Around 1.7 million people in the United States suffer from a Traumatic Brain Injury (TBI) every year, according to the Centers for Disease Control and Prevention (CDC). This type of injury occurs when a sudden external force, such as a blow to the head, causes damage to the brain. While many are aware of the physical and cognitive effects of TBI, the link between TBI and endocrine disorders is not as widely known.
Traumatic Brain Injury (TBI) is a broad term used to describe a wide range of brain injuries caused by a sudden, violent impact or jolt. These injuries can vary in severity and lead to physical, cognitive, and emotional symptoms. One lesser-known complication of TBI is the development of endocrine disorders.
First, let's understand endocrine disorders. Our body releases hormones from specialized glands called the endocrine glands, which control various bodily functions such as metabolism, growth, and reproduction. When there is a problem with the production or function of these hormones, it can lead to an endocrine disorder. Some common endocrine disorders include diabetes, thyroid disorders, and growth hormone deficiencies.
TBI can occur due to a variety of causes, including falls, motor vehicle accidents, sports injuries, and physical violence. These incidents can cause a sudden impact on the head, damaging the brain and surrounding tissues. TBI can range from mild (concussion) to severe, and the severity of the injury can impact the likelihood of developing a related endocrine disorder.
Why Is It Important to Understand the Connection between TBI and Endocrine Disorders?
Discover why understanding the connection between TBI and endocrine disorders is crucial for your health. From hormone imbalances to the impact on brain function, learn the vital link between the two and how it affects your overall well-being:
A person who has experienced TBI may not immediately show symptoms of endocrine disorders. However, regular monitoring of hormone levels can help detect any changes or imbalances early on, allowing for prompt treatment before the symptoms become severe.
TBI can cause endocrine disorders, leading to misdiagnosis and inappropriate treatment. Recognizing this connection helps doctors provide better care.
Endocrine disorders can significantly impact a person's physical and emotional well-being. By understanding the link with TBI and effectively managing the condition, individuals can experience a better quality of life and improved overall health.
Raising awareness about the connection between TBI and endocrine disorders can also help prevent these conditions. For instance, preventive measures such as wearing protective headgear during high-risk activities can reduce the chances of a TBI.
When a TBI occurs, the trauma can disrupt the normal functioning of the endocrine system, leading to a range of disorders. Some common endocrine disorders linked to TBI include:
The pituitary gland, often called the master gland of the endocrine system, regulates hormones for growth, reproduction, and body function. TBI damage is called hormonal imbalances, and symptoms include fatigue, weight gain, and mood changes.
The thyroid produces hormones for metabolism, energy, and temperature regulation. TBI affects brain-thyroid communication, causing dysfunction and symptoms such as weight gain, fatigue, and slow heart rate.
Adrenal glands make stress hormones to manage stress and maintain Blood pressure and electrolyte balance. TBI can harm them, causing fatigue, low BP, and electrolyte issues.
The pituitary gland produces growth hormones for growth and muscle/bone health. TBI can cause growth delays in children and weak bones/muscles in adults.
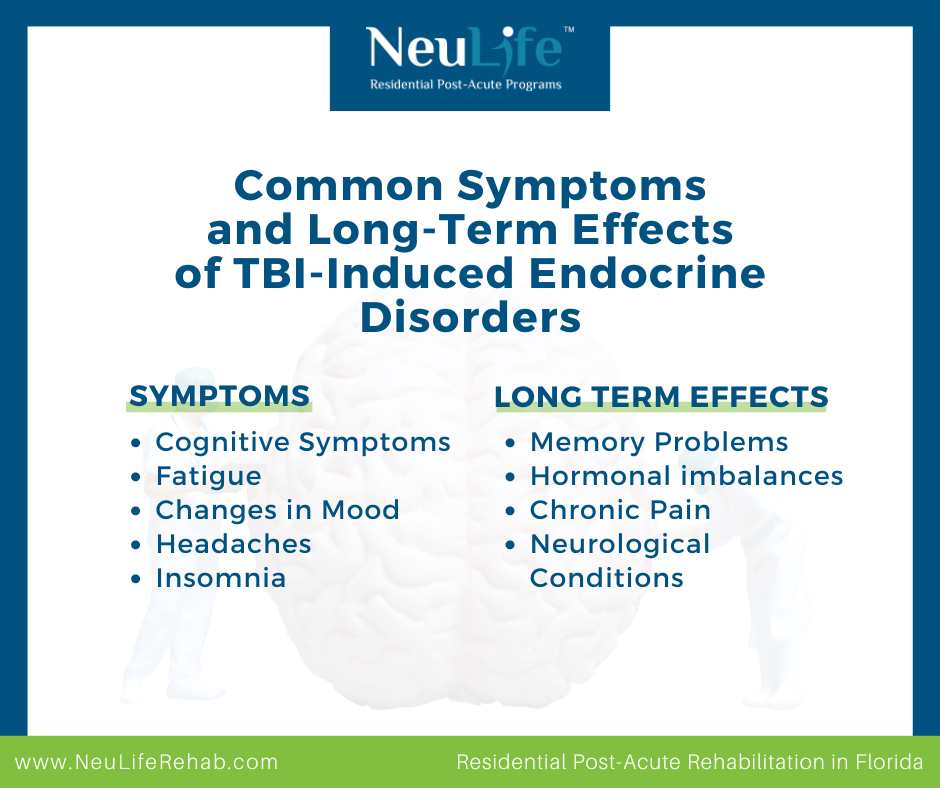
TBI and endocrine disorders can have severe and long-lasting effects on a person's physical and mental health. Although these conditions may seem unrelated, they often occur together and have overlapping symptoms. We will explore the common symptoms and long-term effects of TBI and endocrine disorders and how we can manage and prevent them.
Now, let's look at some common symptoms of TBI and endocrine disorders.
Now, let's dive into the long-term effects of TBI and endocrine disorders, which can have a significant impact on a person's life.
The first step in managing endocrine disorders caused by TBI is accurately diagnosing the condition. This may involve various tests to measure hormone levels and assess the functioning of the pituitary gland. Once diagnosed, the following treatments may be recommended:
The treatment of TBI and endocrine disorders can be complex and may require a multi-disciplinary approach. The primary focus of treatment for TBI is to stabilize the patient and prevent further damage to the brain. This may involve surgery, medication, and rehabilitation to improve cognitive, physical, and emotional function. Once the patient has stabilized, the focus shifts to managing potential endocrine disorders.
If you or someone you know has experienced a TBI, it is essential to be aware of the potential risk of developing endocrine disorders. Here are some tips for managing these conditions:
The connection between TBI and endocrine disorders is undeniable and needs to be understood by both patients and healthcare providers. By recognizing and managing the potential risk of developing endocrine disorders after a TBI, individuals can have better control over their health and lead a fulfilling life.
NeuLife Residential Post-Acute Program provides comprehensive care for individuals with TBI and related complications. Our team of healthcare professionals collaborates to develop individualized treatment plans for neuro rehabilitation, which often include:
NeuLife aims to improve overall health and quality of life for individuals with TBI by providing a holistic approach to recovery. We offer a residential and post acute rehabilitation program designed to help people with brain injuries reintegrate into their communities. Our services are available to patients in Florida and the Southeastern United States. As a top choice for traumatic brain injury rehabilitation care, we welcome anyone affected by such injuries.
If you have questions about traumatic brain injury rehabilitation or any other concerns related to brain trauma, please give us a call to book an appointment today. Additionally, you're invited to schedule a tour of our long-term care facility for traumatic brain injury.
Contact NeuLife today to learn more about our services. Remember, there is always time to start the journey towards recovery.

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Traumatic brain injury (TBI) can significantly disrupt cognitive function, affecting memory, attention, and other essential mental processes.
While physical recovery often takes precedence, cognitive rehabilitation plays a pivotal role in helping individuals regain independence and improve their overall quality of life.

This blog post explores effective techniques to restore memory and attention after a TBI, emphasizing the importance of early intervention and the collaborative nature of the recovery process.
Cognitive rehabilitation is a specialized therapy designed to help people with brain injuries improve their thinking and learning abilities. It focuses on enhancing attention, memory, problem-solving, and other cognitive functions.
While the brain has an incredible capacity for healing, targeted interventions can significantly accelerate recovery.
Research consistently highlights the benefits of early cognitive rehabilitation. The brain is most malleable in the initial months following a brain injury, allowing for optimal neuroplasticity. By starting therapy promptly, individuals can maximize their chances of regaining cognitive abilities.
Here are some of the best cognitive therapies and techniques to improve memory and attention post-TBI.
Memory deficits are a common challenge after a brain injury. Fortunately, various techniques can help individuals enhance their memory function, such as the following:
Memory training exercises are a cornerstone of cognitive rehabilitation for individuals with TBI. These exercises aim to stimulate the brain, improve recall, and enhance overall cognitive function. Here are some examples:
Patients recovering from TBI can also perform practical memory exercises, such as memorizing a grocery list or following a recipe.
Cognitive stimulation involves engaging in mentally challenging activities to improve cognitive function, including memory.

Here are some activities to try:
Start with activities that are challenging but manageable and gradually increase difficulty as cognitive abilities improve.
This involves reviewing information at increasing intervals, which reinforces learning and improves long-term retention.
The core principle of spaced repetition is that information is better retained when review sessions are spaced out over time rather than crammed together. This method takes advantage of the brain's natural learning process, gradually strengthening neural connections.
Mindfulness and meditation have gained significant attention for their potential benefits in various areas of health, including cognitive function.
For individuals with TBI, these practices can offer several advantages, such as improved focus, reduced stress, enhanced emotional regulation, and more. Here are some techniques that patients can incorporate into their daily life:
Practicing a healthy lifestyle not only improves the physical aspects of a patient but also their cognitive abilities. While it won't reverse brain damage, it can significantly enhance brain function and memory.
Attention training exercises are designed to improve focus, concentration, and the ability to filter out distractions. These are crucial for individuals with TBI, as attention deficits are common after brain injury. Here are some common types of attention training exercises:
Sustained attention exercises focus on maintaining attention over a prolonged period. Improving sustained attention is crucial for daily activities and overall cognitive function for individuals recovering from brain injury.
These exercises help individuals focus on specific stimuli while ignoring distractions. Some examples of exercises include:
These exercises challenge the ability to attend to multiple stimuli simultaneously. Specific examples of divided attention exercises include:
These exercises involve shifting attention between different tasks or stimuli.
Attention control involves the ability to direct and regulate one's focus. It's about managing where and how you allocate your mental resources.

Here are some exercises:
A traumatic brain injury can be a life-altering event, affecting not only the individual but also their family and loved ones.
At NeuLife Rehabilitation, we understand the challenges you face, and we are committed to providing the highest level of care and support to help you on your journey to recovery.
NeuLife is a dedicated inpatient facility specializing in post-acute rehabilitation. This means we offer round-the-clock care tailored to your specific needs. Our team of skilled professionals works collaboratively to address the physical, cognitive, and emotional aspects of your recovery. Some of the programs we offer include:
If you or a loved one has suffered a TBI, NeuLife is here to support you every step of the way. Contact us today to learn more about our comprehensive rehabilitation programs.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Spinal cord injuries (SCI) are a complex and often misunderstood medical condition. Various factors, such as accidents, diseases, or genetic disorders, can cause them. Despite the prevalence of SCI, there are many myths and misconceptions surrounding this condition. These misconceptions not only perpetuate damaging stereotypes but they can also hinder the understanding and support of those living with spinal cord injuries.
This blog will debunk common myths and share the truth behind these life-changing injuries. So, let's separate fact from fiction and gain a deeper understanding of the realities of spinal cord injuries.
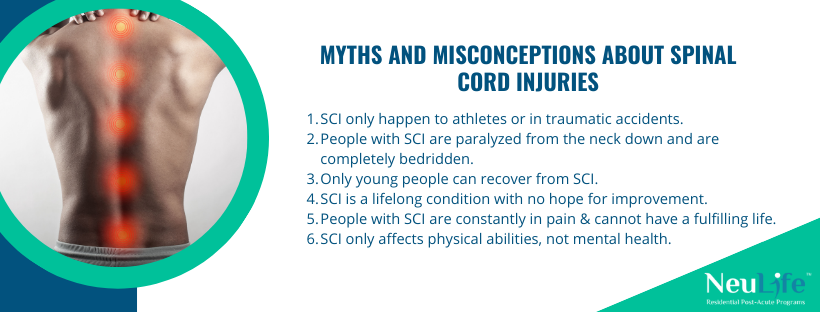
Let’s debunk some of the most common myths and provide factual information about spinal cord injuries.
While it’s true that athletes and individuals involved in traumatic accidents are at a higher risk for spinal cord injuries, they can happen to anyone at any time. The leading cause of SCI is falls, accounting for 31.6% of all cases.
This includes falls from ladders, stairs, and even slips and falls in the home. Other causes of SCI include car accidents, sports injuries, and violence. It’s important to remember that no one is immune to spinal cord injuries.
This is a common misconception that portrays individuals with SCI as wholly immobilized. The truth is that the level and severity of paralysis depend on the location and extent of the injury. For example, a person with a cervical (neck) injury may experience paralysis from the neck down.
In contrast, someone with a lumbar (lower back) injury may have paralysis in the legs but not in the arms. Additionally, individuals with SCI have varying levels of mobility and can lead active and independent lives with the help of assistive devices and therapies.
Another myth about SCI is that only young people have the potential to recover and regain mobility. While it’s true that younger individuals have a higher chance of recovery due to their more robust physical capabilities, that doesn’t mean older individuals can’t make progress as well. With advancements in medical technology and rehabilitation techniques, many older individuals with SCI have shown significant improvement in their condition.
SCI may be a life-changing condition, but it’s not a sentence for a lifetime of suffering with no possibility of recovery. While complete spinal cord healing is impossible, some treatments and therapies can alleviate symptoms and improve function.
These include surgery, medication, physical therapy, and occupational therapy. Additionally, stem cell research and clinical trials show promising results in repairing damaged spinal cords, giving hope for future treatments and potential cures.
Living with SCI may involve chronic pain, but this doesn’t mean that individuals with SCI cannot lead fulfilling and meaningful lives. With proper pain management and support systems, people with SCI can enjoy hobbies, have successful careers, and maintain healthy relationships. It’s also worth noting that every individual’s experience with SCI is unique and shouldn’t be generalized.
Spinal cord injuries not only impact physical abilities but also have a significant impact on one’s mental health. It can lead to feelings of isolation, depression, and anxiety due to changes in lifestyle, limitations, and the constant need for medical care. Addressing mental health is crucial in the overall well-being and recovery of individuals with SCI.
In conclusion, spinal cord injuries are a complex and diverse condition that affects individuals of all ages and backgrounds. While it may be a life-changing event, it’s essential to separate fact from fiction and understand the realities of living with SCI. With advancements in research and technology, there is hope for improved treatments and potential cures. Let’s spread awareness and debunk these myths to create a more inclusive and understanding society for those living with SCI.
SCI can have life-altering consequences for individuals and their families. However, some interesting facts about SCI are worth knowing. Here are some of these facts concisely and informally.
Take control of your recovery journey with NeuLife Rehab, the premier post acute rehabilitation center for spinal cord injuries. Our state-of-the-art facility and individualized treatment plans are designed to help you regain independence and improve your overall quality of life.
In addition to providing exceptional care for spinal cord injuries, we offer various services to support our patients' overall well-being. Our services include:
Don't let a spinal cord injury hold you back. Join our dedicated team of experts and rewrite your story today. Claim your spot in our program now and start on the path to a stronger, healthier you.
Visit our website to learn more about our residential post-acute programs and take the first step towards a healthier, happier life. Let NeuLife be your partner in debunking myths and achieving greatness in the face of a spinal cord injury.

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.

We know that choosing the next step in your recovery from a catastrophic illness or injury is complex. Together, we can help you take the next step.
Contact us with any questions today.