Traumatic brain injury (TBI) can significantly impact a person’s physical, cognitive, emotional, and sensory functions. However, the brain possesses a remarkable ability known as neuroplasticity—the capability to reorganize and form new neural connections after injury.
Through targeted exercises, individuals with TBI can stimulate this plasticity, helping restore lost functions or develop new pathways for daily activities.
This blog post explores 25+ neuroplasticity exercises and strategies to promote brain healing and improve overall well-being.
After a traumatic brain injury, some neural connections may become damaged or lost. This can impair movement, speech, memory, and other critical functions.
Neuroplasticity is the brain’s natural ability to adapt, rewire, and form new neural pathways in response to injury or new learning. This ability is critical in TBI recovery because it enables the brain to:
Simply put, neuroplasticity provides the foundation for healing.
Physical activity is not just beneficial for the body; it's vital for brain health, especially after a TBI. Exercise increases blood flow to the brain, delivering essential oxygen and nutrients. It also stimulates the release of growth factors that support neuron health and neuroplasticity.
Start with short distances on flat, stable surfaces. Focus on maintaining balance and a steady gait. As you improve, gradually increase the duration, speed, and complexity (e.g., walking on uneven ground, inclines, or incorporating head turns).
Begin by standing near a support surface. Practice standing with feet together, then progress to tandem stance (heel-to-toe), and eventually single-leg stands. Hold each position for increasing durations. Using unstable surfaces like foam pads (with supervision) adds difficulty.
This activity targets the brain areas controlling equilibrium and proprioception (sense of body position).
Engage in activities requiring hand-eye or foot-eye coordination. Examples include throwing and catching a soft ball, stacking cones, simple drumming rhythms, or even modified dancing.
These activities force different brain regions involved in motor planning, timing, and sensory integration to work together.
Activities like stationary cycling, swimming, or brisk walking elevate heart rate. Start slowly and gradually increase intensity and duration as tolerated.
Aerobic exercise boosts brain-derived neurotrophic factor (BDNF), a protein crucial for neuron growth and survival, enhancing overall neuroplasticity.
Using light weights, resistance bands, or bodyweight exercises (like sit-to-stands or wall push-ups) helps rebuild the strength needed for daily activities. Focus on controlled movements.
Strengthening muscles improves functional independence and provides sensory feedback to the brain, reinforcing motor pathways.
These practices improve flexibility, range of motion, and body awareness. They often incorporate controlled breathing and mindful movement, linking physical activity with mental focus. Improved body awareness enhances proprioceptive feedback, while the mindful component aids focus and reduces stress, both beneficial for brain recovery.
Cognitive deficits are common after TBI. Exercises targeting memory, attention, problem-solving, and executive functions stimulate the affected neural networks, encouraging them to reorganize and function more efficiently.
Play card-matching games, recall lists of items, or practice remembering sequences of numbers or patterns. Use mnemonic devices (acronyms, visualization) to aid recall. These directly challenge working memory and long-term memory retrieval systems.
Jigsaw puzzles (start with large pieces), crosswords, Sudoku, or word searches engage various cognitive skills. Jigsaws involve visual-spatial skills, while word puzzles target language and logic.
Puzzles require sustained attention, problem-solving, visual scanning, and logical reasoning, activating diverse brain networks.
Numerous apps (e.g., Lumosity, Elevate, Peak) offer games targeting specific cognitive domains like attention, processing speed, memory, and problem-solving. Many adapt difficulty based on performance.
Engaging in something entirely new is a powerful neuroplasticity booster. Consider learning a few phrases in a new language, basic chords on a musical instrument, or simple coding concepts online. Novelty and complexity force the brain to create entirely new pathways and connections.
Work through real-life or simulated problems. Examples include planning a simple daily schedule, figuring out the steps to cook a basic meal, budgeting, or solving logic puzzles. These exercises engage executive functions – planning, organizing, sequencing, and reasoning.
TBI can affect various aspects of communication, including finding words, forming sentences, understanding language, and the mechanics of speech. Targeted exercises help retrain these abilities.
Practice naming common objects around the house or from picture cards. Start with simple items and progress to more complex ones or naming items within a category (e.g., "Name all the fruits you see").
Play games like "I Spy," charades, or description games where you have to describe an object without naming it for someone else to guess. Generate lists of words starting with a specific letter or belonging to a category. These activities actively challenge word-finding (lexical access) pathways.
An SLP or practice partner provides the beginning of a sentence, and you complete it logically (e.g., "To make coffee, I need..."). Gradually increase sentence complexity. This helps rebuild sentence structure and grammatical processing.
Read passages from books, magazines, or newspapers aloud. Focus on clear articulation, appropriate speed, and natural intonation.
Engage in conversations on specific topics with a therapist or communication partner. Practice turn-taking, staying on topic, asking clarifying questions, and using appropriate social language (pragmatics). Role-playing different scenarios can be helpful.
Listen to short stories, instructions, or news segments and answer questions about them. Start with simple yes/no questions and progress to more detailed "wh-" questions (who, what, where, when, why). This exercise targets the brain's ability to process and understand spoken language.
Injury can alter how the brain processes sensory information. Gently stimulating different senses can help retrain these pathways and improve sensory integration.
With eyes closed (if safe), try to identify different objects by touch alone (e.g., keys, cotton ball, sandpaper, coin). Describe textures (smooth, rough, soft, hard). Use therapy putty or stress balls. This enhances tactile processing and discrimination.
Listen to different environmental sounds (birds, traffic, music) and try to identify them. Listen to various music genres or tempos. Try identifying specific instruments in a piece of music. This refines the brain's ability to process and differentiate sounds.
Follow a moving object (like a pen or finger) with your eyes without moving your head. Practice scanning a room or a page systematically to find specific items or information.
Smell distinct, familiar scents like coffee grounds, lemon peel, lavender, or peppermint essential oil (on a cotton ball, not directly inhaled). Try to identify the smell. This stimulates the olfactory pathways, which have strong connections to memory centers.
Mindfully taste small amounts of distinct basic tastes: sweet (sugar), sour (lemon juice), salty (salt water), and bitter (unsweetened cocoa). Focus on identifying the taste sensation. This activates taste receptors and related brain pathways.
TBI recovery can be stressful and emotionally taxing. Mindfulness and resilience techniques help manage stress, improve emotional regulation, and enhance focus – all crucial for healing.
Practice diaphragmatic breathing. Inhale slowly through the nose, allowing the belly to expand, and exhale slowly through the mouth or nose. Focus entirely on the breath.
This activates the parasympathetic nervous system, promoting relaxation and reducing stress hormones that can hinder recovery.
Lie down comfortably and bring gentle, non-judgmental awareness to different parts of the body, starting from the toes and moving slowly up to the head. Simply notice any sensations without trying to change them.
Choose an object (e.g., a flower, a stone, your hand) and observe it intently for a few minutes, noticing details like color, texture, shape, and smell without judgment or analysis. This trains focused attention and present-moment awareness.
Listen to guided recordings or create your own mental scenes of peaceful, calming places (e.g., a beach, a forest). Engage multiple senses in your imagination—what do you see, hear, smell, and feel? This provides a mental escape, reduces anxiety, and can positively influence mood.
Become aware of negative thought patterns related to recovery challenges. Actively challenge and reframe these thoughts into more realistic, constructive, or hopeful ones. For example, change "I'll never get better" to "Recovery takes time, and I am making progress.
This helps manage frustration and maintain motivation, which are vital for sticking with rehabilitation.
At NeuLife Rehabilitation, we understand that true recovery after a traumatic brain injury goes far beyond basic rehabilitation—it requires consistent, specialized care rooted in compassion and clinical expertise.
Our inpatient, post-acute rehabilitation facility is an environment where neuroplasticity can thrive. It is uniquely designed to serve individuals with acquired and traumatic brain injuries, spinal cord injuries, and other complex conditions requiring extensive, round-the-clock support.
Through customized neuro rehab therapy programs, cutting-edge modalities, and a deeply committed interdisciplinary team, we help residents harness the power of neuroplasticity every day—moving them closer to recovery, step by step.
Contact our traumatic brain injury rehabilitation today to learn more.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
The parietal lobe is a critical part of the brain, responsible for sensory perception and integrating sensory information. It is located in the cerebral cortex, the brain's outer layer. The parietal lobe is crucial in various bodily functions, including movement, sensation, and spatial awareness. However, like other brain parts, it is also vulnerable to damage, which can significantly impact an individual's daily life.
This blog post will explore the signs and treatments of parietal lobe injury and how NeuLife can support individuals and their loved ones in neurorehabilitation and recovery.
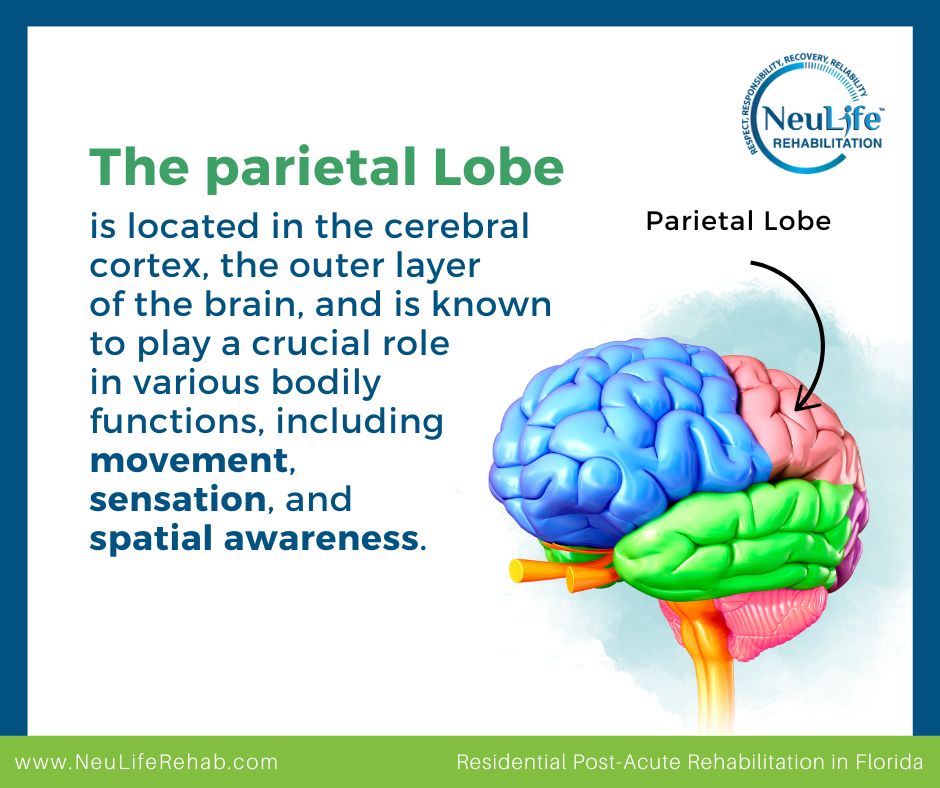
Parietal lobe damage can occur as a result of several factors, including:
This type of injury occurs when a sudden blow or jolt to the head disrupts the brain's normal functioning. In some cases, TBI may damage the parietal lobe directly, affecting its ability to accurately receive and process sensory information.
A stroke occurs when blood flow to the brain is disrupted. A stroke in the parietal lobe can lead to damage and sensory impairments, such as difficulty with touch, sensation, and spatial awareness.
Brain tumors can also damage the parietal lobe. These abnormal growths can press against the brain tissue, leading to various neurological symptoms, including damage to the parietal lobe.
In rare cases, infections in the brain can also cause damage to the parietal lobe. Examples of such infections include encephalitis, meningitis, and brain abscesses. These infections can damage brain tissue, leading to sensory and motor impairments.
Certain neurological disorders can also cause damage to the parietal lobe. Conditions such as Alzheimer's disease, Parkinson's disease, and multiple sclerosis can affect the brain's structure and lead to damage in the parietal lobe.

The symptoms of parietal lobe damage can vary depending on the severity and location of the injury. Generally, the affected individual may experience physical, cognitive, and behavioral changes. Some common symptoms include:
People with parietal lobe damage may experience changes in their sense of touch, taste, smell, vision, and hearing. It can include numbness, tingling, or even loss of sensation in different body parts. The affected individuals may also have difficulty recognizing objects, faces, or colors.
Parietal lobe damage can cause problems with coordination, movement, and balance. It can also make daily tasks like dressing, eating, and writing difficult. The person may have trouble with hand-eye coordination and fine motor skills.
The parietal lobe is responsible for our sense of space and depth perception. Damage to this area can make judging distances, depth perception, and spatial relationships difficult. The person may also have trouble with navigation and get lost easily.
Injuries to the parietal lobe can also cause speech and language difficulties. The person may have trouble understanding spoken or written language, forming words, or finding the right words to express themselves.
The parietal lobe creates and maintains our body image and awareness. Damage to this area can lead to difficulties with body image, such as trouble recognizing one's body parts.
The parietal lobe is vital in integrating and interpreting visual information. Damage to this area can result in changes in perception, leading to distorted or altered views of the external world. The affected individual may have difficulty recognizing familiar objects or faces, leading to facial recognition and object identification challenges.
Parietal lobe damage can also affect a person's behavior and personality. This can include impulsiveness, mood changes, and difficulty with emotion regulation. The affected individual may also struggle with social interactions, become more withdrawn, or have difficulty with empathy.
The treatment options for parietal lobe damage depend on the severity of the injury and the symptoms experienced by the affected individual. In most cases, a combination of therapies and treatments addresses the physical, cognitive, and behavioral changes caused by the damage.
Here are some common treatments used for parietal lobe damage:
Occupational therapy can help individuals with parietal lobe damage relearn daily activities, such as dressing, grooming, and writing. Occupational therapists will also work on improving hand-eye coordination and fine motor skills.
Physical therapy can help individuals with coordination and movement difficulties caused by parietal lobe damage. It includes exercises to improve muscle strength, balance, and coordination.
Speech therapy can be beneficial for individuals with language and communication difficulties. A speech therapist will work on improving language skills, including understanding and using spoken or written language.
Cognitive therapy aims to improve mental functions like memory, attention, and problem-solving skills. It can help individuals with parietal lobe damage regain cognitive abilities and manage any changes caused by the injury.
Behavioral therapy can help individuals with mood or behavior changes caused by parietal lobe damage. It focuses on managing and regulating emotions and improving social interactions.
Managing parietal lobe damage can be daunting and lengthy, but improving and regaining lost abilities is possible with proper care and support. If you or someone you know is facing this condition, do not hesitate to contact NeuLife Rehabilitation of Florida for expert TBI rehabilitation services.
At NeuLife, a trusted post acute rehabilitation center, we specialize in treating parietal lobe damage and understand the unique challenges it presents. Our team recognizes the significance of individualized treatment plans, including specialized stroke patient rehab. With our all-encompassing rehabilitation services, we address the physical, cognitive, and emotional effects of this condition. Our skilled and empathetic therapists collaborate closely with each person to develop a personalized treatment plan that addresses their specific requirements.
To learn more about our services and how we can support your journey to recovery, don't hesitate to reach out to us. For more information about the effects of TBI on different parts of the brain, check out our blog post "What Parts of the Brain are Affected by TBI?" Additionally, our blog "Frontal Lobes Functions" covers tips for managing and recovering from damage to the frontal lobes.
With NeuLife's expertise, you can trust us to provide the best care for parietal lobe damage. Contact us today.

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
We offer a wide range of therapies and treatments, including physical therapy, occupational therapy, speech therapy, and cognitive therapy. At NeuLife, we also place great emphasis on holistic care, incorporating recreational therapy, nutrition management, and mental health counseling, among others, to promote overall physical, mental, and emotional well-being.
In addition to our highly trained staff and individualized care, we also have state-of-the-art facilities designed to provide a comfortable and supportive environment for our clients. Our goal is to support individuals in their recovery journey and help them regain as much independence as possible.
Recovering from a brain injury can be a challenging and transformative journey. It involves managing physical and cognitive changes while adapting to new daily routines. But amid this demanding process, there is a powerful tool that can aid recovery: mindfulness.
Mindfulness is the practice of being fully present in the moment, and it can help patients navigate the emotional, mental, and physical changes that come with brain injuries.
By incorporating mindfulness into recovery routines, individuals can improve their focus, reduce stress, and support their brain's natural healing processes.
Mindfulness is a practice that involves paying attention to the present moment without judgment. It's about being fully aware of your thoughts, feelings, and sensations without getting caught up in them. Essentially, it's a way to train your mind to focus on the here and now.
Mindfulness works by redirecting your attention away from ruminating thoughts or worries and toward the present moment. This can be done through various techniques, such as:
Developing a greater awareness of your thoughts, feelings, and sensations can help you manage the challenges associated with brain injury. Here's how mindfulness can benefit your recovery:
Mindfulness meditation has been shown to support cognitive function, which is crucial after a brain injury. Studies have found that regular mindfulness can improve attention, focus, and memory. This is particularly important for individuals with cognitive challenges accompanying brain injuries.
When practicing mindfulness, the brain's prefrontal cortex—the area responsible for decision-making and concentration—is activated, which can strengthen these cognitive abilities over time. This helps individuals focus on tasks, make decisions with greater clarity, and retain new information during their recovery.
After a brain injury, many people experience heightened anxiety due to uncertainties about their recovery, changes in their abilities, or fear of future injuries.
Mindfulness helps by training the brain to focus on the present moment, reducing the mental habit of ruminating on worries. As a result, stress hormones such as cortisol are lowered, creating a more relaxed state of mind.
Neuroplasticity is the brain’s ability to reorganize itself by forming new neural connections. This ability is essential during recovery after a brain injury, as the brain attempts to adapt and compensate for any damage.
Mindfulness practices have been shown to encourage neuroplasticity by fostering the growth of new neural pathways. When individuals engage in regular mindfulness meditation, they stimulate areas of the brain related to focus, self-regulation, and emotional control.
Brain injuries often lead to difficulty regulating emotions, resulting in sudden mood swings or intense emotional responses.
Mindfulness teaches individuals to observe their emotions without being overwhelmed by them. This practice strengthens the brain's ability to process emotions in a balanced way.
Mindfulness can also support physical healing after brain injury. Studies have shown that mindfulness practices can reduce pain, improve sleep, and boost the immune system.
You can create an optimal environment for your body to heal and recover by cultivating a sense of calm and relaxation.
Various mindfulness techniques can be adapted to suit your individual needs and preferences. Here are some popular practices to consider:
A simple yet effective way to begin mindfulness meditation is through mindful breathing. Here’s how you or your loved one can practice this:
Start with just five minutes a day, gradually increasing the duration as you become more comfortable. This practice helps center the mind and can be incredibly calming when anxiety or frustration arises during recovery.
Body scan meditation is an excellent way to reconnect with your body and bring awareness to any tension or discomfort.
This practice helps improve bodily awareness and can provide a sense of relaxation. Thus making it a valuable tool for individuals experiencing physical discomfort after a brain injury.
Guided meditation apps can be a great starting point for those new to mindfulness. Apps like Headspace, Calm, and Insight Timer offer structured meditation sessions tailored for beginners and specific needs, such as stress relief and sleep improvement.
Incorporating gentle, mindful movement into your routine can particularly benefit individuals recovering from a brain injury.
Practices like yoga or tai chi focus on slow, deliberate movements and emphasize breathing and body awareness. These activities not only help improve balance and coordination but also provide a way to release tension and build strength.
Even if physical limitations exist, modified versions of these practices can be tailored to suit individual needs.
Starting a new practice can be overwhelming, especially when recovering from a brain injury. That’s why it's important to set realistic goals and celebrate small milestones.
Begin with a few minutes of meditation each day and gradually increase the duration as it becomes more comfortable. Remember, consistency is more important than perfection.
On days when it feels challenging to focus, simply sitting quietly and paying attention to your breathing for a few moments can make a difference.
NeuLife Rehabilitation is dedicated to providing top-notch therapy services for individuals recovering from traumatic brain injury (TBI). Besides physical and cognitive therapy, we also believe in the power of mindfulness to enhance brain injury recovery.

Our therapists at our neuro rehabilitation center incorporate mindfulness techniques into their treatment plans. This helps you manage stress, improve cognitive function, and regulate emotions.
If you or someone you know has experienced a brain injury, don't hesitate to reach out to one of the best TBI rehabilitation centers.
Contact NeuLife today to learn more about our post acute rehabilitation.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Shaking or tremors after a head injury can be alarming and disruptive. For many individuals, these involuntary movements significantly impact daily life, causing physical discomfort and emotional distress.
Whether the tremors occur immediately after the injury or develop over time, understanding the underlying causes, symptoms, and available treatments is essential for managing this condition effectively.
In this blog post, we'll explore post-traumatic tremors in detail, breaking down the causes, types, and potential treatment options. By shedding light on this condition, we hope to empower those affected with knowledge and hope for recovery.
Post-traumatic tremors are involuntary, rhythmic muscle movements that often arise after traumatic brain injuries (TBI). These tremors occur due to damage to specific parts of the brain, particularly those involved in motor control, such as the cerebellum, basal ganglia, or thalamus.
Head injuries can disrupt neural pathways that send precise signals to the muscles, leading to uncoordinated or excessive movements. Common causes of post-traumatic tremors include:
Individuals with severe TBIs or those who experience multiple head injuries may be at higher risk of developing tremors. Additionally, a history of neurological conditions such as Parkinson's disease can exacerbate symptoms.
Post-traumatic tremors are characterized by rhythmic shaking or involuntary movements in various parts of the body. Symptoms can vary depending on the severity and location of the brain injury.
Some individuals may also experience secondary symptoms like muscle stiffness, balance issues, or coordination problems, which can further impact daily activities.
Post-traumatic tremors can manifest in different ways depending on the affected brain region.
The most common types include:
This type occurs when the body is at rest and muscles are relaxed. Resting tremors often involve the hands or fingers and can be a sign of damaged basal ganglia.
Action tremors happen during voluntary movements, such as reaching for an object or writing. Subtypes of action tremors include:
Some head injuries can mimic the symptoms of essential tremor, a common movement disorder unrelated to trauma.
This is often slow and intentional, resulting from cerebellar damage. It can affect balance and coordination.
Tremors are just one of many potential movement disorders following a TBI. Other conditions that might cause shaking include:
These disorders often overlap, making precise diagnosis crucial for effective treatment.
A comprehensive evaluation is necessary to identify the type and cause of post-traumatic tremors. Diagnosis typically involves:
Treatment for post-traumatic tremors often requires a multifaceted approach, including medication, therapy, and sometimes surgery.
Medications are often the first line of treatment and can help reduce the severity and frequency of tremors. Some examples include
Rehabilitation plays a crucial role in improving motor function and quality of life. Therapists will help patients adapt to tremors through the following:
For tremors exacerbated by stress, anxiety, or fatigue, the following types of therapies can help.
When other treatments are ineffective, surgical options may be considered:
Doctors often recommend lifestyle changes to complement medical treatment. Some examples include the following:
Recovering from post-traumatic tremors and other effects of a traumatic brain injury requires more than just medical care—it demands a comprehensive approach that addresses both physical and emotional well-being.
At NeuLife Rehabilitation, we specialize in providing the post-acute therapies and support necessary to help individuals regain independence and improve their quality of life.

Our post acute rehabilitation offers care tailored to those living with TBI, spinal injuries, amputations, severe orthopedic conditions, strokes, or neurological disorders. We provide 24/7 care, ensuring that each resident receives the dedicated attention and expert treatment they need.
Contact our neuro rehab today or visit our traumatic brain injury rehabilitation facility.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Stutters are common speech disorders in early childhood, but they can also occur after a traumatic brain injury. Doctors refer to this type of speech impediment as neurogenic stuttering.
For many individuals, experiencing stuttering after an injury can be frustrating, impacting confidence and communication.
Understanding the causes and treatment options for neurogenic stuttering can make a significant difference in recovery.
Neurogenic stuttering is a speech disorder caused by injury or damage to the brain. Unlike developmental stuttering, which appears in early childhood, neurogenic stuttering occurs due to trauma or changes within the brain's structure.
Brain injuries disrupt the neurological pathways responsible for language processing, leading to disruptions in speech fluency. This stuttering may include repeating sounds, prolonging words, or experiencing sudden speech blocks. The condition can affect people of any age and varies widely in severity.
Common symptoms of neurogenic stuttering include:
Neurogenic stuttering may occur immediately after a brain injury or develop later. In addition to affecting communication, neurogenic stuttering can also impact social interaction and personal relationships.
The human brain is a complex network of interconnected regions that work together to produce fluent speech. Key areas involved in speech production include:
Brain injury can damage these areas, disrupting the intricate neural pathways that underlie fluent speech. Here are several factors that can contribute to stuttering after brain injury:
Injury to Broca's area, Wernicke's area, or the motor cortex can directly impair speech production.
Damage to the neural pathways connecting different brain regions can disrupt the coordination of speech movements.
Brain injury can affect cognitive functions like attention, memory, and executive function, indirectly impacting speech fluency.
Anxiety, frustration, and fear of stuttering can exacerbate the severity of the disorder.
Psychogenic stuttering is another form of stuttering that may develop after a traumatic event, though it is less common than neurogenic stuttering.
Unlike neurogenic stuttering, which stems from physical brain damage, psychogenic stuttering arises from psychological stress, anxiety, or trauma. This type of stuttering can occur in people with no prior history of speech disorders.
Psychogenic stuttering may appear suddenly and often coincides with intense emotional trauma or anxiety. For instance, individuals who experience post-traumatic stress disorder (PTSD) following a head injury may develop psychogenic stuttering as part of their reaction to the trauma.
Symptoms are similar to neurogenic stuttering but are often more variable. Some days, the person may experience severe speech interruptions, while other days may show significant improvement.
Treating psychogenic stuttering often requires a different approach than neurogenic stuttering, focusing on addressing the underlying psychological issues through therapy and counseling.
Effective treatment for neurogenic stuttering often involves a multidisciplinary approach, combining speech therapy, medication, and supportive therapies. The primary goal is to help the individual regain fluent speech or develop strategies to manage the condition more comfortably.
Here are some common treatments for neurogenic stuttering:
Speech therapists work closely with patients to develop techniques that improve fluency. This may include:
For individuals with psychogenic stuttering or those who experience stress-related speech issues, CBT can be beneficial. This therapy addresses the anxiety or stress surrounding speech, helping the individual cope with and reduce stuttering symptoms.
In some cases, medications may assist in reducing symptoms associated with neurological issues. While there is no specific drug to cure stuttering, medications for managing anxiety, mood disorders, or neurological conditions may provide relief and help improve communication.
Support groups offer individuals a space to discuss their experiences and gain confidence in communicating. Counseling can be especially valuable for those dealing with psychogenic stuttering or anxiety after a brain injury.
Some individuals benefit from devices that alter auditory feedback. These devices, worn in the ear, can help the speaker hear their voice differently, reducing stuttering frequency.
Stuttering after a brain injury can be complex, but with the proper support and treatment plan from NeuLife Rehab, improvement is possible.

NeuLife Rehabilitation is a premier provider of comprehensive rehabilitation services for patients who have suffered from traumatic brain injury (TBI) and its resulting conditions. We provide programs to suit each patient's needs—from post acute rehabilitation to speech therapy.
Our neuro rehabilitation center has a state-of-the-art facility and a highly skilled team of therapists, neurologists, and rehabilitation specialists. We provide unparalleled care to help patients regain independence, improve quality of life, and achieve their recovery goals.
NeuLife Rehabilitation isn’t just a place to recover; it’s a place to rebuild, renew, and regain independence.
Contact one of the best TBI rehabilitation centers today to learn more.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Traumatic brain injury (TBI) can have a profound impact on a person's life, both physically and mentally. One of the less common but potentially debilitating symptoms that can arise after TBI is paranoia.
Paranoia is characterized by persistent and unfounded suspicions or distrust of others. It can significantly impair a person's relationships, quality of life, and overall well-being.
Read on below and learn about the causes, symptoms, and treatment options for paranoia in TBI patients.
Paranoia is a persistent and unfounded belief that others are out to harm or deceive you. It involves excessive suspicion, mistrust, and vigilance, even when there is no evidence to support these beliefs.
Paranoia can be a symptom of various mental health conditions, including schizophrenia, bipolar disorder, and post-traumatic stress disorder (PTSD).
Paranoia after TBI is a complex issue with multiple contributing factors. While the exact mechanisms are not fully understood, several theories have been proposed:
Traumatic brain injury can cause damage to various brain regions, including those involved in memory, perception, and emotional processing. This damage can disrupt the normal functioning of these areas, leading to distorted thoughts and perceptions.
TBI can disrupt the balance of neurotransmitters—the chemical messengers that facilitate communication between brain cells. Imbalances in neurotransmitters, such as dopamine and serotonin, have been implicated in the development of paranoia.
Pre-existing mental health conditions, such as anxiety or depression, can increase the risk of developing paranoia after a brain injury. Additionally, the stress and emotional trauma associated with a TBI can contribute to the development of paranoid thoughts.
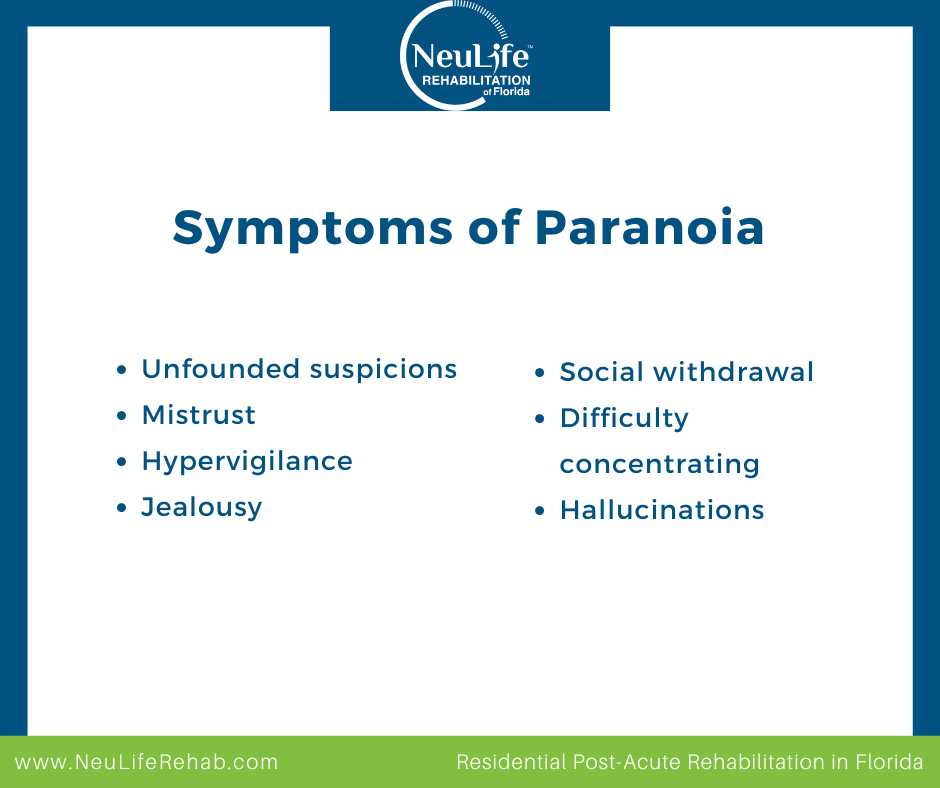
Paranoia in patients with TBI can manifest in various ways, and the severity of symptoms can vary greatly. Some common symptoms include:
Paranoia can also lead to social isolation, difficulty maintaining relationships, and problems with employment. Patients may be constantly on guard, making it difficult to concentrate or relax. This can also lead to increased stress and anxiety, further exacerbating symptoms.
Paranoia and anxiety can sometimes overlap, making it difficult to distinguish between the two. However, there are some key differences:
Paranoia also shares some similarities with other mental conditions, particularly schizophrenia, bipolar disorder, and borderline personality disorder.
Diagnosing TBI-related paranoia involves a comprehensive evaluation by a qualified neuropsychologist.
They may perform several diagnostic exams, such as neurological exams, neuropsychological testing, and mental health assessment.
After a comprehensive evaluation, they can develop a personalized treatment plan for the patient.
The treatment for paranoia in TBI patients may involve a combination of approaches, depending on the severity of symptoms and the individual's needs. This includes the following:
Medications can be used to help manage symptoms of paranoia, such as antipsychotics and antidepressants.
Cognitive-behavioral therapy (CBT) is often effective in treating paranoia by helping patients identify and challenge negative thought patterns.
Support groups can provide a sense of community and emotional support for individuals with TBI and paranoia. Connecting with others who have similar experiences can help reduce feelings of isolation and stigma.
Making lifestyle changes, such as getting enough sleep, exercising regularly, and managing stress, can also help improve symptoms of paranoia.
Providing support to a loved one experiencing paranoia after TBI can be challenging. However, it's important to remember that your support can make a significant difference. Here are some strategies:
Learn as much as you can about TBI and paranoia. This can help you better understand your loved one's experiences and provide more effective support.
Here are some helpful communication strategies you can do to make your loved one feel supported:
A healthy and supportive environment can help your loved one with TBI-related paranoia feel more comfortable, confident, and hopeful. Here’s how you can do that:
Encouraging your loved one to seek professional help and undergo therapy can be a valuable tool for managing paranoia and improving overall quality of life.
A therapist can help your loved one develop coping strategies, challenge negative thought patterns, and build healthy relationships.
If you or a loved one is experiencing paranoia after a brain injury, it’s crucial to seek specialized care from professionals who understand the complexities of this condition, like the medical team at NeuLife.

NeuLife Rehabilitation is one of the best brain injury rehabilitation centers and a leading provider of post-acute rehabilitation. We offer comprehensive, personalized care tailored to the unique needs of TBI patients.
Our multidisciplinary team includes experts in neurology, psychology, physical therapy, and rehabilitation who work together to create individualized treatment plans.
At NeuLife, we go beyond treating the injury itself—we address the full spectrum of challenges associated with TBI, including cognitive impairments, behavioral issues, and emotional health. Our holistic approach ensures that patients not only recover physically but also regain confidence and stability in their daily lives.
Contact us today and learn more from our neuro rehabilitation team.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
According to the most recent data, there were approximately 214,110 Traumatic Brain Injury (TBI)- related hospitalizations in 2020. With this alarming statistic in mind, it is crucial to make informed decisions when it comes to seeking rehabilitation for a loved one who has suffered a brain injury.
Knowing what factors to consider and what qualities to look for in a rehabilitation center can be challenging at such a difficult time. However, choosing a suitable facility can make all the difference in a patient's recovery and transition back home.
This article will discuss the key components that make a brain rehabilitation center suitable and how they can contribute to achieving desired patient outcomes.
The right brain rehabilitation center should offer multiple forms of therapy to ensure recovery. The best rehabilitation centers provide but not limited to:
Look for a traumatic brain injury rehabilitation center with an experienced team that utilizes the latest technologies in their field. The goal is to reduce the patient's limitations, maximize independence, and offer advancement to return to a rewarding life.
Sometimes, amenities can be a factor in choosing the proper post-acute rehabilitation. Though amenities never replace quality medical care, they can offer patients additional comfort and entertainment that are important for healing.
Some of the best brain injury rehabilitation centers offer the following for their patients to add to their overall well-being:
Additionally, patients should regularly have access to staff. The team should include doctors, occupational therapists, physical therapists, counselors, dieticians, case managers, nurses, and support staff available to assist patients in excelling through their stay.

Finding a trusted center for optimal care is crucial if you’re looking for a brain rehabilitation facility. These key factors will ensure you or your loved one receives the best care and support for a successful recovery.
The people working at a brain rehabilitation center are super important. They need to be experts in their field. This means they should be well-trained and know much about brain injuries and how to treat them. The staff includes doctors, nurses, therapists, and counselors.
Why It’s Important:
Experts know the best ways to help patients heal. They can create personalized plans that fit each patient’s needs.
Everyone’s brain injury is different, which means each person's treatment should be different, too. A good brain rehabilitation center makes a unique plan for each patient. This plan should consider the type of injury, the patient's age, and goals.
Why It’s Important:
A personalized plan helps patients recover faster and more effectively. It focuses on the specific areas that need healing.
Many types of therapies can help someone with a brain injury, including:
Why It’s Important:
Different therapies target different problems. Having a variety of options means that all aspects of recovery are covered.
Modern technology can make a big difference in brain rehabilitation. This includes things like virtual reality, robotics, and specialized computer programs.
Why It’s Important:
Advanced technology can speed up recovery, make therapy more effective, and make therapy more engaging and fun for patients.
The rehabilitation center's environment should be comfortable and welcoming. Patients need to feel safe and at home. This includes clean, spacious rooms, good food, and relaxing areas.
Why It’s Important:
A comfortable environment helps patients feel better emotionally. When patients are happy and relaxed, they can focus more on their recovery.
Families play a crucial role in the recovery process. A good brain rehabilitation center involves the family in the treatment plan and provides training and support to help family members understand the patient’s needs.
Why It’s Important:
Family support can motivate patients and make them feel loved. It also helps families know how to care for their loved ones once they return home.
Patients and their families need to understand the brain injury and the recovery process. A good rehabilitation center provides education and training on these topics. This includes information on what to expect, how to manage symptoms, and ways to support recovery at home.
Why It’s Important:
Knowledge is power. Understanding the injury and recovery process can reduce fear and anxiety. It also helps patients and families feel more in control.
Recovering from a brain injury is not just about physical healing. It’s also about emotional healing. A good brain rehabilitation center offers counseling and emotional support for patients and their families.
Why It’s Important:
Emotional support helps patients cope with the challenges of recovery. It can reduce feelings of depression and anxiety, which can improve overall recovery.
Recovery doesn’t stop when a patient leaves the rehabilitation center. Ongoing support is crucial. This includes follow-up appointments, continued therapy, and support groups.
Why It’s Important:
Post-rehabilitation support ensures that patients continue to make progress and don’t feel alone in their recovery journey.
The best way to measure a rehabilitation center’s success is by examining its patients' outcomes. A good center should have a track record of helping patients improve and reach their recovery goals.
Why It’s Important:
Positive outcomes show that the center’s methods are effective. It gives patients and families confidence in the care they are receiving.
If you or a loved one needs brain rehabilitation, consider NeuLife Residential’s Post Acute Rehabilitation Programs. Neulife Rehabilitation is one of Florida's largest neuro rehabilitation centers. We offer comprehensive, quality medical care, superior therapy modalities, and amenities to honor the patient's well-being. Our care is individualized to the needs of every patient.
At our neurological rehabilitation center, we specialize in rehabilitating a wide range of injuries and have the experience you can trust. We encourage you to learn more about our facility and programs.
If you have any questions, we are here for you! Call us or schedule a tour to learn how we can support you or your loved one through brain rehabilitation. We look forward to being a part of your recovery!

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Imagine yourself reaching for a familiar word, the one that perfectly captures your thoughts. But suddenly, it's gone, replaced by a frustrating blankness. This is the daily reality for many people living with aphasia, a language disorder that arises from brain injury.
Aphasia disrupts a person's ability to communicate, affecting speaking, listening, reading, and writing. While strokes are a leading cause, brain injuries from accidents, tumors, or infections can also trigger aphasia.
Aphasia disrupts the brain's complex network that is responsible for language processing. Different areas of the brain manage various aspects of language, such as comprehension, expression, and retrieval of words. Damage to these areas can lead to a variety of communication difficulties and other challenges, such as:
The human brain is a marvel of interconnectedness, and language processing is no exception. Several key regions work in harmony to enable us to speak, understand, read, and write.
Unfortunately, brain injuries, whether from strokes, TBIs, or other causes, can disrupt this delicate network in several ways:
A blow to the head or a blockage in a blood vessel can directly injure specific language processing areas, leading to particular types of aphasia depending on the location of the damage.
The intricate web of connections between different brain regions is vital for language fluency. Injury can sever these connections, making it difficult for information to flow smoothly between language centers.
Brain injury often triggers inflammation and swelling, which can temporarily impede communication even without direct damage to language centers.
Aphasia isn't a single condition; it manifests in various forms depending on the location of the brain injury. Here's a breakdown of some common types:
Broca’s aphasia, also known as non-fluent or expressive aphasia, affects the ability to produce fluent speech. People with Broca's aphasia may speak in short, telegraphic phrases and struggle to find words. Comprehension, however, is often relatively intact.
Wernicke's aphasia disrupts language comprehension. Speech may sound fluent but nonsensical, with misused words and jumbled sentence structures. Wernicke’s aphasia is also known as fluent aphasia or receptive aphasia.
This type primarily affects word retrieval. People with anomic aphasia know what they want to say but have difficulty finding the exact word. They may use circumlocutions (descriptive phrases) or resort to gestures to communicate.
This is the most severe form of aphasia, and it significantly affects all aspects of language—speaking, understanding, reading, and writing.
While there's no single cure, promising treatment options can significantly improve communication skills and overall well-being.

Let's delve into the tools therapists use to help people with aphasia rebuild their language abilities.
This method aims to reawaken dormant language skills in the brain. Therapists may use techniques like picture naming, sentence completion, or melodic intonation therapy (using melody and rhythm to improve speech production).
The brain is remarkably plastic, meaning it can reorganize itself to compensate for damage. Therapists may use techniques that target undamaged brain regions to take on new language-processing functions.
This can involve tasks like practicing alternative ways to express oneself or using visual cues to support comprehension.
For some individuals, particularly those with severe aphasia, AAC tools can bridge the communication gap.
These tools can range from low-tech options like picture boards to high-tech speech-generating devices that allow individuals to communicate by selecting pre-programmed phrases or even typing words that are then spoken aloud by the device.
This intensive therapy approach focuses solely on verbal communication. Therapists restrict the use of alternative communication methods like gestures or writing, forcing the brain to rely on spoken language. Studies suggest CIAT can be effective for some individuals in improving language production.
Cognitive rehabilitation focuses on retraining and strengthening cognitive skills that might be impaired after brain injury. Some examples of techniques used include:
Family members and caregivers play a vital role in supporting someone with aphasia. Here are some ways to help:
Family and friends can be a powerful force in supporting someone with aphasia. Their patience, understanding, and willingness to adapt communication styles can significantly impact the recovery journey.
Brain injury can be a life-altering event, leaving individuals facing a complex journey of recovery. At NeuLife Rehab, we understand the unique challenges associated with brain injury and its associated disorders.

NeuLife Rehab is one of the best TBI rehabilitation centers in the state. Our team comprises highly trained therapists with extensive experience treating brain injury and its consequences. We have a deep understanding of this condition and its various forms, allowing us to create individualized treatment plans that address each patient's specific needs.
Our neuro rehabilitation facility goes beyond traditional therapy, offering a holistic approach that incorporates speech therapy, cognitive rehabilitation, physical therapy, and occupational therapy.
Contact our post-acute rehabilitation center today to schedule a consultation. Let us help you rediscover the power of communication and rebuild a fulfilling life.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Imagine waking up after an accident and feeling like a stranger inhabits your own body. This can be a reality for some individuals who have experienced a traumatic brain injury (TBI).
Beyond the physical challenges, TBI can also lead to significant changes in personality, leaving patients and loved ones grappling with a new normal.
This blog post explores the reasons why personality shifts occur after TBI. We'll explore the impact of brain damage on various functions, the emotional toll of the injury, and how these factors combine to create personality changes.
A traumatic brain injury (TBI) can lead to many physical problems like impaired memory, frequent headaches, dizziness, and balance issues.
However, TBI may also cause personality changes, and this is something that many patients grapple with. Here's a breakdown of some frequently observed shifts, along with relevant statistics:
Thus, a psychological evaluation following a TBI is essential to facilitate a better treatment plan for the patient.
Scientists cannot pinpoint the exact reason why traumatic brain injuries can change one's personality. But here are two primary reasons why these changes happen:
Experts in neuro-rehab widely believe that TBI affects the intricate connections between the cerebral cortex and the limbic system. The cerebral cortex helps the brain process memory, cognition, perception, and awareness.
The limbic system, located below the cerebral cortex, is the center for brain functions like emotions and behaviors.
A TBI can be a life-altering event. Patients may experience frustration, depression, and anxiety as they cope with physical limitations, cognitive difficulties, and a changed sense of self. These emotions can manifest as changes in behavior or personality.
Studies suggest that up to 77% of patients can develop mood disorders (e.g., depression, anxiety problems) within a year of experiencing a traumatic brain injury.
Some experts in post-acute rehabilitation also believe that patients who experience TBI are already in an exceptionally stressful situation. People respond to any form of extreme trauma in the body differently.
Some TBI survivors may end up doing or saying things they don’t mean, while other patients become more emotional than they were before they suffered a TBI.
Some patients present heightened aggression and quickly become frustrated and short-tempered. For others, the changes could be subtle and less significant.
It's challenging for many patients to recover from a traumatic brain injury. It's important, however, to recognize the emotion and understand why these changes happen to prevent a full-blown mental illness.

Here's how you can offer support to someone navigating these challenges:
Create a safe space for open and honest communication. Talk to them about your concerns in a supportive and non-judgmental way.
Knowledge is power. Learning about TBI and its effects on personality can help you be more patient and empathetic. Families or friends around the patient must also be sensitive to these changes.
Support from a professional is also paramount, as therapy and neuro-rehab may help the patient manage and correct these personality changes. Some treatment options to help patients manage their personality changes after TBI include:
This therapy helps patients identify and change negative thought patterns contributing to emotional dysregulation. CBT can be highly effective in managing symptoms like irritability, anxiety, and depression.
This type of therapy helps patients relearn social skills that may have been affected by the TBI. It can teach them to understand social cues, interpret facial expressions, and maintain healthy relationships.
In some cases, medication may help manage co-occurring mental health conditions like depression or anxiety that can contribute to personality changes. It's essential to work with a doctor to determine the best course of medication management.
Connecting with others who understand the challenges of TBI can be incredibly helpful. Support groups can provide a space for patients to share their experiences, learn coping mechanisms, and feel less alone.
Therapy can help families learn how to communicate effectively and support their loved ones.
A traumatic brain injury can leave a lasting impact not only on physical abilities but also on a person's personality and emotional well-being.

NeuLife Rehabilitation understands the multifaceted challenges of TBI recovery. That’s why we are dedicated to helping patients regain their independence and navigate the full spectrum of TBI’s effects, including personality changes.
Our experienced team specializes in different types of rehabilitative programs, such as:
Schedule a consultation with our team and learn how our personalized approach to TBI rehabilitation can empower you on your journey to recovery.
NeuLife is a residential post-acute rehab facility specializing in brain injury rehabilitation. As one of the best post-acute rehabilitation centers in Florida, its program includes:
Beautifully situated on 43 acres in Mount Dora, Florida, its inpatient rehab facility comprises over 60,000 square feet and contains 54 private rooms or suites. If you would like more information about NeuLife Rehabilitation services, please contact us.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
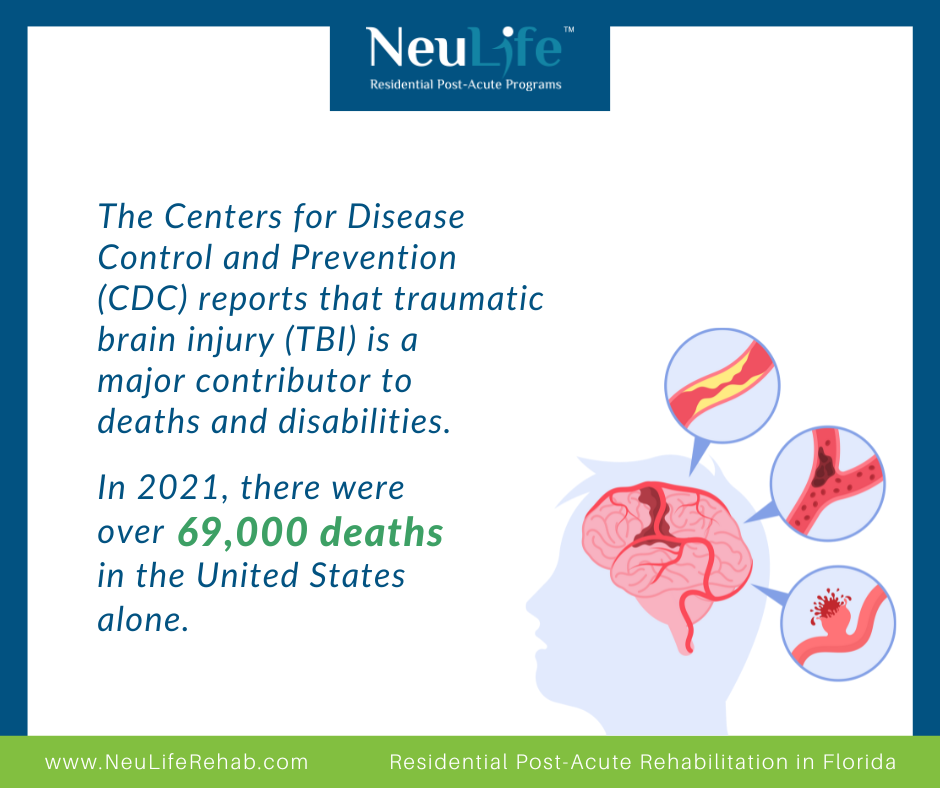
According to the Centers for Disease Control and Prevention (CDC), traumatic brain injury (TBI) is a significant cause of death and disability. There were over 69,000 TBI-related deaths in the United States in 2021. This type of injury can significantly impact a person's physical, cognitive, and emotional functioning, decreasing quality of life.
Fortunately, occupational therapy (OT) has proven effective in helping individuals with brain injury regain functional independence and improve their overall well-being. In this blog post, we will explore how occupational therapy helps brain injury and the specialized programs offered at NeuLife Residential for optimal recovery.
Before delving into how occupational therapy can benefit individuals with brain injury, it is essential to understand what brain injury is and the impact it can have on a person. A brain injury occurs when there is a disruption in the brain's normal functioning, either due to a blow or jolt to the head or a penetrating injury.
The severity of the injury can range from mild to severe and can affect different areas of the brain, leading to various physical, cognitive, and emotional impairments. These impairments may include movement, speech, memory, attention, emotional regulation, and problem-solving difficulties.

Occupational therapy is a holistic approach that focuses on helping individuals participate in meaningful activities or occupations that are important to them. In the case of brain injury, occupational therapists work with individuals to help them regain their functional abilities and independence in daily activities.
Here are some ways in which occupational therapy can help people with brain injury:
One of the primary goals of occupational therapy for TBI is to help individuals achieve and maintain functional independence. This means being able to perform daily tasks and activities without assistance.
Occupational therapists work closely with TBI patients to assess their physical, cognitive, and psychological abilities and develop personalized treatment plans accordingly. These plans may include activities to improve self-care skills, such as dressing, grooming, and eating, as well as community reintegration activities, such as using public transportation or managing finances. By addressing these functional tasks, OT helps individuals regain independence and control over their lives.
TBI can lead to various cognitive impairments, such as memory loss, difficulty concentrating, and impaired decision-making abilities. Occupational therapy can help individuals with TBI by providing exercises and activities to improve these cognitive skills. For example, therapists may use memory games, puzzles, and problem-solving activities to help patients regain cognitive abilities and function more independently.
After a TBI, individuals may find engaging in activities they previously enjoyed challenging. Occupational therapy can help individuals identify meaningful activities that align with their interests and abilities and work towards participating in them again. Individuals with TBI can improve their overall quality of life by finding purpose and enjoyment in activities.
TBI not only affects an individual's physical and cognitive abilities but can also significantly impact their emotional well-being. Dealing with the aftermath of a traumatic injury can be overwhelming and can cause feelings of frustration, anxiety, and depression. Occupational therapists are trained to address these emotional issues, providing support and guidance for individuals to cope with their emotions, reduce stress, and improve their mood and overall well-being.
TBI can lead to secondary complications, such as muscle weakness, joint stiffness, and decreased range of motion. Occupational therapists use various techniques, including therapeutic exercises and manual therapy, to prevent these complications and help individuals maintain their physical function. They also educate patients on strategies and techniques they can use to manage these symptoms independently.
Brain injury can often cause social isolation and difficulty participating in community activities. Occupational therapists can help individuals identify and overcome barriers hindering their participation, making it easier for them to reintegrate into their communities.
The impact of TBI extends beyond the individual, affecting their family members and caregivers. Occupational therapists can involve family members in therapy sessions to provide support and education on assisting their loved ones in their recovery. This includes teaching techniques for managing challenging behaviors and addressing any adjustments needed in the home to accommodate the individual's needs.
Knowing which provider is the best fit for you can be overwhelming with so many options available. Here are some tips for choosing the right occupational therapy provider.
At NeuLife Residential Post-Acute Programs, we understand that each individual with a brain injury has unique needs and goals. Our specialized post-acute programs are designed to provide tailored, evidence-based treatment to help individuals achieve their maximum rehabilitation potential.
Here are some of the specialized programs we offer to individuals with brain injury:
If you or a loved one has experienced a brain injury, it is vital to seek rehabilitation services to promote optimal recovery. At NeuLife Residential, a top-tier neuro rehabilitation center, we have a team of experienced and dedicated professionals committed to helping individuals with brain injuries reach their full potential.
Schedule a tour today or contact us at 352-675-2059 to learn more about our post-acute programs and take the first step towards a more independent and fulfilling life. We are here to support you on your journey to recovery.
***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Have you or a loved one experienced a traumatic brain injury (TBI)? If so, you might be familiar with the physical and emotional challenges that can follow. But did you know TBI can also cause psychosis in some cases?
Psychosis is an alarming complication that can significantly impact recovery and quality of life. In this blog post, we will delve into the complex link between TBI and psychosis, exploring the risk factors, underlying mechanisms, treatment options, and the importance of early recognition.
Psychosis is a mental health condition where an individual experiences a break from reality, often manifesting as hallucinations (seeing or hearing things that aren't there) and delusions (false beliefs that are firmly held despite evidence to the contrary).
A person can develop psychosis due to a combination of factors (e.g., genes, mental illness). However, if one sustains a traumatic brain injury, their chances of developing psychosis significantly increase.
The onset of psychosis after TBI can vary widely, from days to decades after the injury. However, it is generally delayed, with some studies reporting an average onset of several years.
The severity of the injury, location of brain damage, genetic predisposition, and other individual factors can influence the likelihood of developing psychosis.
Research suggests that traumatic brain injury can increase the risk of developing psychosis, although the exact reasons are still under investigation. Several factors appear to play a role in this complex connection:
More severe TBI cases, particularly those involving damage to specific brain regions like the frontal and temporal lobes, seem to be associated with a higher risk of psychosis.
Brain injury can disrupt the delicate balance of neurotransmitters in the brain, particularly dopamine, which plays a crucial role in psychosis.
The inflammatory response triggered by brain injury can further contribute to neurotransmitter imbalances and brain dysfunction, potentially leading to psychosis.
Individuals with a family history of psychosis may be more susceptible to developing the condition after traumatic brain injury.
Early identification of psychosis symptoms is vital for timely intervention and improved outcomes. Following a head injury, be vigilant for the following signs:
If you or someone you know experiences these symptoms after a traumatic brain injury, seeking professional help from a mental health specialist is crucial.
Diagnosing psychosis after brain injury can be challenging due to overlapping symptoms with other post-TBI conditions.
A comprehensive evaluation involving a thorough medical history, neurological examination, and psychological assessment is often required.
Treating psychosis after traumatic brain injury requires a multi-faceted approach that addresses both the psychotic symptoms and the underlying brain injury. Here are the main treatment options:
These medications are the primary treatment for psychosis. They work by modulating neurotransmitters in the brain, particularly dopamine, which plays a crucial role in psychotic symptoms. Some examples of medications include:
The choice of medication depends on individual factors like age, medical history, and severity of symptoms.
Psychotherapy can be beneficial in helping individuals understand and cope with their psychotic experiences, develop coping skills, and improve their overall functioning.
One example is cognitive behavioral therapy, which is often used to help individuals challenge and reframe their delusional beliefs and manage hallucinations.
Other therapies like supportive therapy, family therapy, and social skills training can also be helpful.
In some cases, other medications may be used along with antipsychotics, depending on the specific needs of the individual.
A supportive and structured environment is crucial for individuals with psychosis after brain injury. This may involve psychoeducation for the individual and their family, social support groups, vocational rehabilitation, and assistance with daily living activities.
In rare cases, ECT may be considered for individuals with severe or treatment-resistant psychosis, especially when there is a significant risk of harm to themselves or others.
The optimal treatment plan is typically individualized and may require adjustments over time based on the individual's response to treatment and any changes in their symptoms.
When life takes an unexpected turn due to a traumatic brain injury or other catastrophic events, regaining your independence and quality of life becomes the utmost priority.

At NeuLife Rehabilitation, we understand the unique challenges you face and offer comprehensive, compassionate care to help you on your journey to recovery.
We also address co-occurring conditions holistically, providing comprehensive mental health support and pain management strategies to enhance your overall well-being.
Our team of experienced physicians, therapists, and nurses specializes in various therapies and services tailored to your needs. This includes:
and more.
If you or a loved one is struggling with the aftermath of a traumatic brain injury, NeuLife Rehabilitation is here to help.
Contact us today at 352-668-2035 to learn about our programs.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Are you or a loved one facing the challenges of managing a spinal cord injury? In the United States alone, around 17,700 new spinal cord injury cases are reported each year. This injury can occur from various causes, including car accidents, falls, and violent acts. When one's spinal cord is affected, it can lead to paralysis, neurological issues, and limited mobility.
Coping with these challenges can be overwhelming, but fear not, as there is light at the end of the tunnel. This blog will explore the common challenges faced after a spinal cord injury and provide practical tips on managing and overcoming them. So, let's dive in and learn how to navigate these obstacles together.
Spinal cord injury happens when there's damage to the spinal cord, which is a bundle of nerves running from the brain down the back. There are two primary types of SCI: complete and incomplete. Complete SCI results in a total loss of sensation and motor function below the injury site.
At the same time, incomplete SCI allows movement and sensation below the affected area. These injuries can have life-altering consequences, affecting mobility, sensation, and bodily functions. Raising awareness about SCI is vital to promote prevention measures and support those living with these challenges.

SCI can bring life-altering challenges, impacting various aspects of daily life. From mobility to emotional well-being, individuals with SCI cope with a unique set of challenges daily that demand resilience and support. Let’s dive into the common challenges faced by people with spinal cord injuries and shed light on their journey towards overcoming them.
One of the primary challenges for individuals with SCI is mobility limitations. Damage to the spinal cord can result in partial or complete paralysis, affecting movement and coordination. Simple tasks like walking, reaching, or transferring from one place to another become daunting challenges.
Independence is precious to everyone, but maintaining it can be an ongoing battle for those with SCI. From relying on assistive devices like wheelchairs to needing assistance for daily activities, the loss of independence can be emotionally taxing and frustrating.
SCI often brings a host of health complications, including respiratory issues, bladder and bowel dysfunction, and pressure sores. Managing these health concerns requires constant vigilance, specialized care, and sometimes invasive medical interventions.
The financial impact of SCI can be overwhelming. Medical expenses, adaptive equipment costs, home modifications, and ongoing therapies can quickly accumulate. Moreover, many individuals with SCI may need help securing employment or maintaining their previous earning potential, further exacerbating financial strain.
Living with SCI can take a toll on one's emotional and mental well-being. Coping with the sudden change in circumstances, adjusting to a new way of life, and facing societal stigma can lead to feelings of isolation, depression, and anxiety. Building a solid support network and accessing mental health resources are crucial for emotional resilience.
Navigating an inaccessible environment is a constant challenge for individuals with SCI. From inaccessible buildings to lack of transportation options, barriers to accessibility hinder their participation in various aspects of life, including education, employment, and social activities.
SCI can lead to social isolation due to physical limitations, accessibility barriers, and societal misconceptions. Feeling disconnected from friends, family, and community can contribute to feelings of loneliness and depression. Building inclusive communities and fostering social support networks are essential for combating social isolation.
After a suspected spinal cord injury, quick action is critical. First, call emergency services for professional help. Next, keep the person still and avoid moving them unless necessary to prevent further damage. If they're not breathing or their heart isn't beating, CPR might be required.
If the patient is unconscious but breathing, gently support the head and neck to align them. Don't give them anything to eat or drink. Stay calm and reassure them until help arrives. Immediate care can make a big difference in their recovery, so acting fast and staying focused is crucial.
Treating spinal cord injuries can be challenging due to the complex nature of the spinal cord itself. The spinal cord is delicate, and damage to it can lead to permanent disability. Each injury is unique, making it hard to find a one-size-fits-all solution. Limited understanding of how the spinal cord works adds another layer of difficulty. Additionally, regenerating damaged nerve cells is a big challenge for medical science. All these factors combined make treating spinal cord injuries a tough nut to crack.
Spinal cord injuries can change lives in a blink, but hope exists for recovery. Whether someone can bounce back from a spinal cord injury depends on various factors. Firstly, the severity of the injury plays a significant role. Minor injuries heal with time and therapy, while severe ones may have lasting effects—secondly, timely medical care matters. Quick intervention can prevent further damage and improve chances of recovery.
Moreover, the individual's determination and attitude are crucial. Rehabilitation programs, including physical therapy and counseling, offer support and guidance. While not everyone may fully recover, progress is possible. Advances in medical research continually provide new treatments and hope for those affected. So, while the journey may be challenging, staying hopeful and exploring all avenues for recovery is essential.
When a person faces such an injury, coping becomes crucial. Coping means finding ways to handle challenges and live the best life possible. Let's explore some ways people cope with spinal cord injuries.
Getting prompt medical attention is crucial after an SCI. This might involve surgery, rehabilitation, and ongoing medical care to manage symptoms and prevent complications.
Many individuals with SCIs undergo physical therapy to regain strength, mobility, and independence. These exercises can also help prevent muscle atrophy and improve overall well-being.
Learning new ways to perform everyday tasks is essential for those with spinal cord injuries. This might involve using assistive devices, modifying living spaces, and mastering adaptive techniques to maintain independence.
Dealing with an SCI can take a toll on mental health. Seeking support from friends, family, support groups, or mental health professionals can provide invaluable emotional support and coping strategies.
Understanding one's rights and advocating for accessibility and inclusivity is vital for individuals with SCIs. Education about SCI-related issues empowers individuals to navigate challenges and access necessary resources.
Keeping up with advancements in SCI research, treatments, and technologies can offer hope and new possibilities for those living with spinal cord injuries.
Getting through life after a spinal cord injury presents challenges but with the right strategies and support, many can be managed effectively. Individuals can enhance their quality of life and regain independence by focusing on adaptive techniques, seeking resources, and building a solid support network.
While setbacks may occur, perseverance and a positive mindset can pave the way for a fulfilling life post-injury. By staying informed and proactive, those affected can continue overcoming obstacles and thriving in their recovery and adaptation journey.
From relearning daily activities to regaining independence, our comprehensive rehabilitation programs at NeuLife cater to individuals with spinal cord injuries, providing personalized care every step of the way.
Whether you're seeking rehabilitation for brain injury, spinal cord injuries rehabilitation, or other neurological conditions, NeuLife - a top neuro rehabilitation facility - is here to support your recovery journey. As a leading post-acute rehabilitation center, we prioritize your well-being and progress.
Don't let a spinal cord injury hold you back from living life to the fullest. Take the first step towards a brighter future with NeuLife. Contact us today to learn how we can help you overcome common challenges after spinal cord injury and embark on recovery. Let us guide you towards a life of renewed strength and vitality.

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.

We know that choosing the next step in your recovery from a catastrophic illness or injury is complex. Together, we can help you take the next step.
Contact us with any questions today.